Browse through our Medical Journals...
Neurosarcoidosis presenting with delusions
*Efrain Mendez MD, *Brian Ladds MD, **Harold Tanenbaum MD MBA, #Abdul Mondul MD, #Rajinder Garg MD, #B Kanna MD MPH FACP
Affiliations:
Lincoln Medical and Mental Health Center
Affiliated with Weill Medical College of Cornell University
* Department of Psychiatry
** Department of Radiology
# Department of Internal Medicine
ABSTRACT
In sarcoidosis, neurological involvement is frequently accompanied by systemic disease. Common manifestations of neurosarcoidosis include cranial nerve palsy and pituitary dysfunction. Neurosarcoidosis presenting with mainly psychiatric symptoms is rare. We report the unusual presentation of neurosarcoidosis with delusions and without concurrent systemic involvement in an established case of sarcoidosis, along with review of literature.
MESH key words: Sarcoidosis; Delusions; Neurologic Manifestations; complications
INTRODUCTION
Sarcoidosis is a chronic, multisystem disorder of unknown cause characterized by an accumulation of T-cell lymphocytes and mononuclear phagocytes, non-caseating epithelioid granulomas, and derangements of the normal tissue architecture in affected organs.
Neurological involvement is an uncommon initial presentation of sarcoidosis, even less so with only psychiatric symptoms, being in such cases more difficult to diagnose and treat. (1)
We present an interesting case of grandiose delusions due to neurologic involvement in a patient with pre-existing sarcoidosis.
CASE DESCRIPTION
Our case is a 37-year-old African-American male, brought to the emergency department (ED) by his wife with a complaint that, “he is having memory problems and claims to be a famous pop singer”. The wife also reported that “he was not himself” and he has been “sleeping too much for two months” along with frequent memory lapses. He had been sent back from work because of excessive sleepiness and also had few episodes of fainting spells recently. She became concerned when the patient, after waking up that morning, began “making funny faces” and patient stated that she was a popular contemporary television character. Later, the patient recollected having the thoughts, but could not explain why he was thinking that he and his wife were celebrities.
There was a previous history of substance abuse, including cocaine and marijuana seven years ago. There was no personal or family history of psychiatric illness. Medical history included childhood onset bronchial asthma, diet controlled type 2 diabetes mellitus, systemic sarcoidosis including initial pulmonary involvement diagnosed by bronchoscopy and panhypopituitarism on thyroid supplements and hydrocortisone for the past 11 months. There was no history of joint, skin or eye involvement related to sarcoidosis since diagnosis. A history of two episodes of syncope, one a week before and another 17 months ago were also noted. The patient also reported feeling tired, lethargic and loss of libido.
At the time of the psychiatrist’s interview in the ED, no psychomotor agitation or retardation was noted. His mood was normal, although his affect was constricted, but appropriate. There were no disorders of thought in form or content. He denied any perceptual disturbances. He denied suicidal or homicidal ideation. His judgment, insight and impulse control were good.
Mental status examination revealed an oriented, slightly drowsy individual. Initial blood pressure was 115/75 mm Hg; heart rate 59 per minute and body temperature was normal. Pulmonary, cardiac, joint, skin, cranial nerves & peripheral nerve examination was normal. There were no signs of meningeal irritation. A limited ophthalmologic examination of visual fields, visual acuity, pupillary reflex and ocular muscles was normal.
Chest roentgenogram showed no abnormalities typical of sarcoidosis. The urine toxicology screening was negative. A 12-lead electrocardiogram showed normal sinus rhythm, left anterior fascicular block and non-specific repolarization abnormality in lateral chest leads.
Gadolinium enhanced brain magnetic resonance imaging (MR) demonstrated mildly enlarged ventricles, dense enhancement of the basal cisterns and parafalcine leptomeninges with adjacent bi-frontal edema that were consistent with neurosarcoidosis. Additional differential diagnosis possible included tuberculosis, although considered unlikely given the clinical data. Concurrent brain magnetic resonance angiography revealed intermittent stenosis of the bilateral A-1 segments suggestive of angiitis. An electro-encephalogram showed a non-specific pattern of generalized slowing, and sporadic bi-temporal spikes but without propagation of the activity.
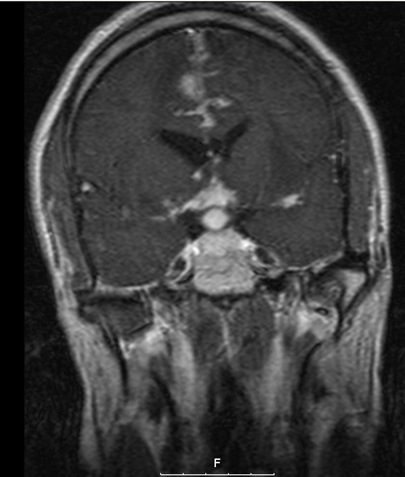
Figure 1. Gadolinium -enhanced coronal T1 MR Image illustrating supra-sellar enhancement suggestive of sarcoidosis
Laboratory evaluation revealed low levels of serum thyroid stimulating hormone 0.0047 microIU/mL(normal range 0.35 – 4.8 microIU/mL); free thyroxin 0.71 ng/dL ( normal range 0.9 – 1.9 ng/dL); follicular stimulating hormone 0.9 U/mL ( normal range 1.0 – 14.0 U/mL); and luteinizing hormone < 0.07 U/L ( normal range 1.5 – 9.3 U/L) consistent with pan-hypopituitarism.
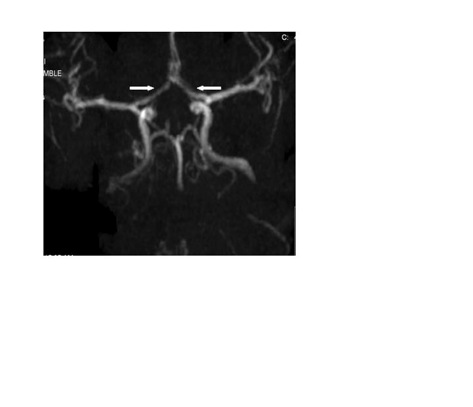
Figure 2. Coronal MRA revealing bilateral A1 segment narrowing (arrowheads point towards the segments)
Levothyroxine dose was escalated from 100 micrograms to 112 micrograms and high dose prednisone 60 mg once daily was started for treatment of neurosarcoidosis. During hospitalization, the patient had fewer episodes of drowsiness without delusions that resolved completely in about one week. The patient was discharged on oral systemic steroid and thyroid supplements to a physical rehabilitation facility.
DISCUSSION
Neurosarcoidosis is present in only 5% of sarcoidosis patients. Manifestations due to neurosarcoidosis are sub-acute to chronic in onset and appear usually within the first 2 years of the illness. Neurosarcoidosis presents as uni- or bilateral peripheral facial nerve palsy (52%), polyneuritis or polyneuropathy (24%), meningeal involvement (24%), or Guillian-Barre syndrome (5%). (2) Neuroendocrine dysfunction occurs with hypothalamic parenchymal inflammation. Death due neurosarcoidosis occurs in about 18% of cases. In our patient, there were no nerve palsies. He had radiological evidence of hypothalamic involvement, communicating hydrocephalus due to lepto-meningeal sarcoidosis and neuroendocrine dysfunction.
Early in the disease process, the basilar meninges are most commonly involved leading to cranial neuropathies and hypothalamic dysfunction. From the meninges, the inflammatory process extends into the brain and spinal cord through Virchow-Robin perivascular spaces. The severity of the acute inflammatory reaction correlates with the clinical picture and chronic fibrosis can lead to irreversible neurologic damage. As described in literature, our case had typical meningeal involvement leading to hypothalamic dysfunction.
Psychiatric manifestations in neurosarcoidosis are unusual (3) and may be in the form of delirium, psychosis, mood disturbances, cognitive impairment, and personality changes. Involvement of dopaminergic neurons in the nucleus accumbens bilaterally has been implicated in such conditions. (4) Our patient presented with grandiose delusions of acute onset due to neurosarcoidosis as reported in the few cases in literature. Of the 5% of sarcoid patients who develop neurosarcoidosis, only 20% will display psychiatric symptoms. (5) The diagnosis of neurosarcoidosis is difficult given the unusual clinical presentation of only psychiatric symptoms. A high index of suspicion is required for recognition of such an atypical presentation in neurosarcoidosis.
A gadolinium enhanced magnetic resonance imaging scan of the brain is the most sensitive radiological procedure for suspected CNS involvement. (6) On magnetic resonance neuro-imaging, neurosarcoidosis predominantly involves the basal leptomeninges and less commonly presents as parenchymal nodules. (7) The ventricular enlargement noted in our patient is due to meningeal involvement resulting in communicating hydrocephalus. Vascular involvement due to spread from the leptomeninges through the Virchow robin spaces leads to granulomatous angitis that resulted in the A1 segment stenosis seen on our patient’s MRA. Although the findings noted on MRA are manifestations highly suggestive of neuro-sarcoidosis, these can also be seen in other conditions such as primary angitis, collagen vascular diseases and atherosclerosis. However, given the history and clinical presentation makes other diagnoses very unlikely.
Treatment of neurosarcoidosis with psychiatric presentation is high dose potent corticosteroids. A prompt clinical response occurred in our case after initiation of therapy with no recurrent delusions or drowsiness. In general, once clinical response occurs, corticosteroids can be gradually tapered and complete withdrawal may be attempted. Relapse in clinical symptoms requires a repeat course of high-dose steroid treatment. Treatment related toxicity can be significant and must be monitored regularly. (8) Other available treatments for those who are remain unresponsive or intolerant to high dose steroids, are immunosuppressive agents and immuno-modulators, including cyclosporine, azathioprine methotrexate, and most recently anti-cytokines. Surgery is rarely indicated and is reserved for cases that present with lesions producing mass-effect that do not respond to medical treatment, as in patients with acute hydrocephalus. In severe recalcitrant cases, low dose radiation may be useful. (9)
Patient using corticosteroids also present with psychotic symptoms that need to be differentiated from symptoms of neurosarcoidosis. Psychiatric symptoms with steroid use are usually mild and appear at the beginning of therapy and tend to wane (10). In view of acute psychotic symptoms in our case on chronic low dose steroids, the radiological findings and the need for urgent steroid therapy in neurosarcoidosis, a decision to administer steroids was taken. The prompt and definitive improvement of neuro-psychiatric symptoms noted in our patient during high-dose steroid therapy supports the diagnosis of neurosarcoidosis. Such response to therapy although not usual, has been reported in other cases. (11)
Somnolence and sleep disorders such as narcolepsy and cataplexy have been described in patients with neurosarcoidosis. (12) In our case, somnolence and syncope was also noted. The likely explanation could be sarcoid infiltration of lateral hypothalamus with reduction in hypocretin cells as it has been shown in patients with narcolepsy (13) On the other hand hypothyroidism due to panhypopituitarism could also explain the sleepiness, tiredness and loss of libido described by the patient.
CONCLUSION
Our case illustrates that neurosarcoidosis can present with neuro-psychiatric manifestations including delusions, in addition to pan-hypopituitarism and hypothalamic disturbances. It is important to differentiate this condition from psychotic symptoms related to chronic steroid use and other neuro-psychiatric syndromes. Knowledge and awareness of this complication of systemic sarcoidosis is important to internists and psychiatrists in the appropriate management of such patients.
REFERENCES
1. Harrison’s Principles of Internal Medicine, 15th Edition 2001 (vol 2). Chapter 18:1973
2. Sharma, OP. Neurosarcoidosis: A personal perspective based on the study of 37 patients. Chest. 1997; 112: 220-28.
3. Allen RK, Sellars RE, Sandstrom PA. A prospective study of 32 patients with neurosarcoidosis. Sarcoidosis Vasc Diffuse Lung Dis. 2003; 20(2):118-25.
4. James A., Richard JM, Rogers et al. Neurosarcoidosis and Delirium. Psychosomatics 2005; 46:148-150
5. Joseph RB; Sondralyn MF; Morris JF et al. Neurosarcoidosis as a Cause of Refractory Psychosis: A Complicated Case Report
Am J Psychiatry 1998; 155: 1106-08
6. Lury KM, Smith JK, Matheus MG, Castillo M.. Neurosarcoidosis--review of imaging findings.Semin Roentgenol. 2004; 39 (4):495-504.
7. Miller DH et al. Magnetic resonance imaging in central nervous system sarcoidosis. Neurology. 1988; 38(3):378-83.
8. Gullapalli D and Phillips LH, Neurologic Manifestations of Sarcoidosis, Neurologic Clinics; 20(1) Neurologic Manifestations of Systemic Disease, 2002: 59-83. Available at < (http://www.sciencedirect.com/science/article/B6X3H-4950200-5/2/2bcf524a25eb1eec6d1949dde73157b5)>
9. Bruns F, Pruemer B, Haverkamp et al. Neurosarcoidosis: an unusual indication for radiotherapy. British Journal of Radiology 2004; 77: 777-79
10. Brown ES, Chandler PA. Mood and cognitive changes during systemic corticosteroid therapy. Primary care companion, J Clin Psychiatry .2001; 3:1
11. Reed LD, Abbas S, Markivee CA, Fletcher JW. Neurosarcoidosis responding to steroids. Am. J. Roentgenol. 1986; 146: 819-821
12. Rubinstein I, Gray TA, Moldofsky H, Hoffstein V. Neurosarcoidosis associated with hyper somnolence treated with corticosteroids and brain irradiation. Chest. 1988; 94(1):205-6
13. Hungs EM, Mignot E. Hypocretin/orexin, sleep and narcolepsy. Bioessays. 2001(5):397-408.
Corresponding Author information:
Balavenkatesh Kanna MD, MPH, FACP
Assistant Professor of Clinical Medicine
Weill Medical College of Cornell University, New York
Associate Program Director of Internal Medicine & Associate GME Director
Lincoln Medical & Mental Health Center
234 E 149th Street Bronx NY
Copyright Priory Lodge Education Limited 2008
First Published August 2008
priory Useful links
Click
on these links to visit our Journals:
Psychiatry
On-Line
Dentistry On-Line | Vet
On-Line | Chest Medicine
On-Line
GP
On-Line | Pharmacy
On-Line | Anaesthesia
On-Line | Medicine
On-Line
Family Medical
Practice On-Line
Home • Journals • Search • Rules for Authors • Submit a Paper • Sponsor us
All pages in this site copyright ©Priory Lodge Education Ltd 1994-


