Browse through our Journals...
Psych-technology: A Systematic Review of the Telepsychiatry Literature
Ashraf Melaka and Sisira Edirippulige
Centre for Online Health
The University of Queensland
Level 3, Foundation Building
Royal Children’s Hospital
Herston 4029
Australia
Summary
Recent advances in Information and Communication Technology (ICT) have created opportunities to assist in providing alternate solutions to the delivery of quality psychiatric services. This study sets out to review the literature related to the use of ICT in the psychiatry field. The study was conducted using electronic databases such as Medline, PubMed, Google Scholar, Web of Knowledge, PsycINFO and Embase covering the period 1996 to March 2008. The focus of the study was on reviews including studies reporting cost-effectiveness, patient outcomes, technology implementations and services, applications in different geographical settings (developed and undeveloped countries), the use of telepsychiatry in Australia and the barriers to the practice of telepsychiatry. These studies were classified as randomised control trials, evaluation studies and review studies. Fifty-three articles were identified that fulfilled the inclusion criteria. Results from the randomized controlled trials analyzed have demonstrated that telepsychiatry treatment has equivalent efficacy to face-to-face consultation.
Synchronous technologies applied in psychiatry practice include: videoconferencing, telephony and online chat programs. Asynchronous technologies include: online support groups, email and self-help groups. The application of telepsychiatry has increased in developed countries such as: USA, Canada and Europe. Telepsychiatry has also been widely used in a number of programs to service rural Australian regions. A lack of application and evolvement of telepsychiatry in developing countries was evident in this review study as well as a lack of economic studies comparing the costs associated with conventional psychiatry services against the costs associated with telepsychiatry services.
This review study has shown the potential of telepsychiatry services to assist in the provision of effective mental and psychiatric care.
Introduction
Psychiatry is the diagnosis, treatment and prevention of mental health conditions (NHS, 2008). Mental health services often are inadequate in remote areas with few specialty providers. Providing traditional psychiatry services has been negatively impacted by many factors including: lack of workforce, lack of accessibility and costs associated with patient travel.
The use of telemedicine is perceived as a potential alternative to improve these services since the majority of interaction and intervention is conducted visually or verbally.
Wootton defines telemedicine as the practice of medical care using interactive, audio, visual and data communications (Wootton, 2006).
The use of Information and Communication Technologies to provide mental health services is known as telepsychiatry. Telepsychiatry as defined by Wootton et al is “the delivery of health care and the exchange of health information for purposes of providing psychiatric services across distances” (Wootton, 2003 p3). The term telepsychiatry is an all-encompassing term for any form of ICT medium used in the delivery of psychiatric services. It is believed that telepsychiatry and e-mental health are becoming widely used in psychiatric diagnosis and treatment (Wootton, 2003:pxiii). Other terminologies used in literature interchangeably with the term telepsychiatry include E-mental health and telemental health. E-mental health as defined by Wootton relates to mental health services provided through any form of electronic medium, most commonly via the Internet or telephone (Wootton, 2003 p3). Telemental health as defined by Smith and Allison is delivering mental healthcare at a distance (Smith & Allison, 1998).
The objective of this study is to systematically review the literature related to the effective use of ICT in psychiatry.
The study will examine:
• Current telepsychiatry services practiced and their application through synchronous and asynchronous technologies.
• Geographical practice settings including Australia.
• Reported barriers and limitations affecting telepsychiatry applications.
Methods
Search Strategy
The review study is of the telepsychiatry literature from 1996 to March 2008 using Medline, PubMed, Google Scholar, Web of Knowledge, PsycINFO and Embase. The author reviewed the article titles and abstracts to decide their relevance and application to the field of telepsychiatry. The searches used in these databases are shown in Table 1. In addition, some articles were identified by reading the reference lists of other published articles. Volumes of the Journal of Telemedicine and Telecare (vol. 2, 1996 to vol. 2, 2008) were checked manually. The author also acquired valuable knowledge through reviewing telemedicine and telepsychiatry books authored by Richard Wootton.
Selection Criteria
The primary selection criteria for this study were to investigate randomized control trial studies in telepsychiatry. Well designed and executed trials, particularly randomized controlled trials provide the most reliable evidence for inclusion in any systematic literature review. This was followed by research of a variety of literature sources relating to the application of telepsychiatry including evaluation and review studies. Evaluation studies incorporated research associated with: feasibility, acceptability, cost effectiveness and evaluation of services in various locations around the world. Review studies incorporated literature reviews on telepsychiatry as well as current standards and guidelines used in this field. This study only focuses on the application of technology in the field of psychiatry and excludes literature associated with the application of technology in other health disciplines. Titles and abstracts of the studies identified by the search strategies in table 1 were read to determine their potential eligibility for the review. The full articles were then assessed for relevance.
Inclusion criteria
| Step | Search Term |
| 1 | Telepsychiatry or E-mental Health OR Telemental health |
| 2 | Telemedicine OR Teleconsulting OR Video Conferencing OR telephony OR telephone Or synchronous communication OR asynchronous communication OR Online Consultations OR Self-help Groups OR Application OR online groups |
| 3 | Australia OR Queensland OR South Australia OR NSW OR Victoria OR Western Australia |
| 4 | Cost OR cost-effectiveness OR success OR failure OR barriers OR limitations OR Challenges OR Implications OR Legal OR Ethical OR Privacy OR Confidentiality |
| 5 | 1 and 2 |
| 6 | 1 and 3 |
| 7 | 1 and 4 |
| 8 | 1 and 2 and 3 |
| 9 | 1 and 3 and 4 |
| 10 | 1 and 2 and 4 |
Table 1 – Literature Search strategy
Studies included reported cost-effectiveness outcomes, patient outcomes, technology implementations and services, applications in different geographical settings (developed and undeveloped countries), application in Australia, clinician satisfaction and telepsychiatry barriers. Included studies were classified as randomised control trials, evaluation studies and review studies. Technology studies included were classified as synchronous applications (use of video-conferencing, telephony and online chat programs) and asynchronous applications (use of e-mail, online support groups and self-help groups). Psychiatry disciplines included: child and adolescent, paediatric psychiatry, forensic psychiatry, veteran’s health psychiatry and mental health.
Results
The search terms specific to telepsychiatry and their combinations yielded 193 references from MEDLINE and over 200 references from PubMed. Altogether 93 papers were chosen for more detailed analysis, of which 53 fulfilled the inclusion criteria. These 53 papers are outlined in Table 2 in appendix A. A manual search of the Journal of Telemedicine and Telecare yielded 3 more papers. The author also reviewed in detail the book Telepsychiatry and e-mental health by Wootton et al. (Wootton, 2003)
There were four randomized control trial studies on the application of telepsychiatry. Nine papers were found on the evaluation of telepsychiatry programs specifically in Australia with emphasis on servicing of rural districts. There were thirty-three papers selected relating to evaluation of telepsychiatry programs in various international locations around the world. Fifteen papers found were review studies of the telepsychiatry literature. Amongst these reviews and evaluations were studies from Canada, USA, Canary Islands, India, Pakistan, Europe and the UK. Studies found related to cost, feasibility and application of telepsychiatry services.
Table 2 summarises the findings of the 53 articles analysed into 3 categories:
1. The types of technology applications used in psychiatry practice (synchronous and asynchronous),
2. The application of telepsychiatry internationally and in Australia
3. The limitations and barriers affecting telepsychiatry practice.
| Study Category | Description | No of Studies |
| Types of Technology used in psychiatry services | Application of synchronous technologies | 38 |
| Application of videoconferencing | 22 | |
| Application of the telephone in telepsychiatry | 12 | |
| Application of synchronous communication using online chat programs and forums | 6 | |
| Application of asynchronous technologies | 15 | |
| Application of telepsychiatry internationally and in Australia | Application of telepsychiatry in developed countries (USA, Canada, Europe, Australia) | 51 |
| Telepsychiatry in developing countries | 2 | |
| Application of telepsychiatry only in Australia | 9 | |
| Limitations and barriers in telepsychiatry practice. | Universal guidelines to govern telepsychiatry practices | 2 |
| Ethical and legal factors in telepsychiatry | 10 |
Table 2 – Study categories
Research Quality
Study designs are essential to consider when conducting systematic literature reviews. As in any health research discipline, large randomised controlled studies are the gold standard (Egger, Smith and Altman, 2001). Other study designs to be considered included case-controlled studies, cohort studies, retrospective studies and review studies.
In this systematic literature review the number of randomised controlled trials found was small (only 4 were analysed). A number of other study designs were analysed. These were categorised into 2 categories:
Evaluation studies: feasibility studies on the application of telepsychiatry.
Review studies: literature review studies on application of telepsychiatry.
An assessment of the quality of the RCT studies was conducted (Appendix B). This assessment provided reassurance that these studies were quality contributions in the current available telepsychiatry literature.
Discussion
A total of 53 articles were reviewed in this study. Findings from these articles are presented in three sections below: The types of technology applications used in psychiatry practice (synchronous and asynchronous), the application of telepsychiatry internationally and in Australia, the limitations and barriers affecting telepsychiatry practice.
Technologies
Application of synchronous technology
This study investigates the use of synchronous communication technologies in particular videoconferencing, telephony and online chat programs. These have been the most widely used in telepsychiatry practice. Disciplines and clinical applications where these forms of telepsychiatry have been most beneficial include: services to correctional facilities (Zaylor et al, 2001, Leonard, 2004), veteran’s health (Godleski, 2004), forensic services (Zaylor et al, 2001), pediatric services (Starling, 2006, Boydell, 2004), geriatric medicine (Jones, 2001), mental health (Merkel, 2004, Hogenbrick, 2006), psychological testing and neuropsychological assessment (Hilty, 2004). Child and adolescent services have been another field, which is receiving much attention in the telepsychiatry literature (Starling 2003, Myers 2007, Myers 2008).
Videoconferencing is considered the central technology currently used in telepsychiatry, because it permits live, two-way interactive, full-color, video, audio, and data communication (De las Cuevas, 2006). The Canary Islands telepsychiatry program in Spain is one example of many recent programs that have been established to provide psychiatric service to rural regions (Pesämaa 2004, Mielonen 2002). From the same program in the Canary Islands, a randomized control trial (RCT) demonstrated that telepsychiatry treatment has equivalent efficacy to face-to-face consultation in psychiatric treatment (De las Cuevas, 2006). Another RCT in Canada (O’reilly 2008) illustrates that psychiatric consultation and short-term follow-up, when delivered by telepsychiatry, can be as effective, as when it is provided face to face. Videoconferencing has also been beneficial in the training, education and supervision of students in the field of psychiatry and in linking academic centers with rural areas and clinics for teaching and educational demonstrations. (Hilty, 2004, Simpson, 2001).
The use of the telephone has also been integral in telepsychiatry communication and has been a precursor to the more sophisticated distance technologies currently used in practice. Due to accessibility, the telephone has become a standard tool for psychiatrists in scheduling, consultation, payment and crisis management (Mallen et al, 2005) The telephone has also been widely used as a means of interaction in psychotherapy. In Australia, the kids help line service is the countries only free, confidential and anonymous, telephone counseling service specifically for young people aged between 5 and 25. Counselors respond to more than 10,000 phone calls each week about issues ranging from relationship breakdown and bullying to sexual abuse, homelessness, suicidal thoughts, and drug and alcohol usage. Since 1991 more than 5.2 million telephone and online chat sessions (audio and visual) have helped children seeking Kids Help Line's support (Kids Help Line, 2006). The study by VandenBos and Williams of 600 psychologists in the USA reported 98% providing psychiatric services by telephone (VandenBos & Williams, 2000). The telephone is also commonly used amongst psychiatrist for referrals, emergency care, consultation and education, individual psychotherapy and clinical supervision (Mallen et al, 2005).
Online and virtual community chat programs offer a forum whereby people interact with others including psychiatry professionals, sharing their experiences and conditions. The benefits of synchronous communication in online group and chat psychotherapy include the real-time, live interaction whereby response is immediate. The use of video/web vision technologies assist in maintaining the visual and real-time interaction. Questions are answered interactively allowing collaboration and further discussion. This form of practice can be very helpful in achieving therapeutic goals (Tate 2004). One of the most useful aspects of online counseling is the ability to use new technologies to conduct assessments, evaluations, and therapy in remote locations (Mallen, 2008). The kids helpline service in Australia also provides an online counseling service. This service provides one-on-one real time contact with a counselor. This service is available during specified times in the day. Users are encouraged to make regular appointments to meet online with counselors using this service (Kids Help Line, 2006).
Telepsychiatry applications offer a cost-effective alternative to traditional psychiatry interaction however the challenges confronted by using these applications include limited bandwidth, quality of service and security (Hilty 2004).
Application of asynchronous technology
Asynchronous communication includes non-real time interaction such as email groups and user forums. The use of any asynchronous interaction should only be used for non-urgent consultations as this form of interaction is non real-time. Types of information transferred can be in the form of data, audio, still images or video recordings.
The uses of email and online support groups such as doctor online (Jonson 2002) and the Samaritan organisation (Feinichel, 2001) have proven to be effective forms of telepsychiatry services. Online social support groups have been used extensively and have become useful for a range of disorders including; sexual abuse (Barak, 2007), suicide and depression (Barak, 2007, Houston et al, 2002) cancer (Meier, 2007), and disabilities (Kroll, 2007). In general, results have found that online groups provide therapeutic support similar to face-to-face formats (Tate 2004). Houston et al examined the effects of Internet based support groups for depression and found that participants reported considerable support from their computerized interactions (Houston et al 2002) Online support groups are also becoming very useful as motivational tools to weight loss and dealing with obesity. The use of Internet self-help groups also offers a unique form of support based on mutual understanding between patients and psychiatrists. Benefits of self-help groups include: providing social and emotional support to users, information and experience sharing as well as practical assistance and advice from psychiatrists. Other benefits include 24-hour availability, accessibility from users location and anonymity. Tate and colleagues (Tate, Jackvony, & Wing, 2003; Tate, Wing, & Winett, 2001) developed an Internet self-help behavioural treatment program for obesity in California. This program included behavioural lessons posted on the web site each week, reporting of self-monitoring information via web-based diaries, opportunities for group support via electronic bulletin boards, and participant–therapist interactions via e-mail. Results of this study suggested that weekly e-mail communication with a weight loss counsellor significantly improved weight losses over a one-year program.
Geography of practice including Australia
Application in different geographical settings
This study found that the application of telepsychiatry has increased in developed countries such as: USA, Canada, Europe and Australia. Fifty one of the studies analyzed were conducted in these countries highlighting the wide adoption of these technologies in practice. The results of this study also demonstrate the lack telepsychiatry use in developing countries. This is not uncommon to the general telemedicine experience in the developing world. “There has been little practical experience with telemedicine of a direct clinical kind in the developing world which contains 80% of the world’s population.” (Vasallo et al, 2004). Only 2 studies found in this research were relating to telepsychiatry clinical practice in developing countries (India and Pakistan). In India, the Society for Administration of Telemedicine and Healthcare Informatics (SATHI) offered telepsychiatry services to tsunami affected persons in Nagarpattinam district in the state of Tamil Nadu (Majumdar, 2007). The study by Rahman in Pakistan referred to the training and education of existing staff. The study demonstrated a practical method for training and supervising colleagues in Pakistan from a distance (Rahman, 2006).
The published literature clearly shows that telepsychiatry for the developing world is at a very early stage and there is a need for the delivery of telepsychiatry to serve developing nations. This is due to the large population density within these developing nations. The development of evaluation studies and clinical trials (both in the developed and developing worlds) are fundamental to providing the foundation for implementing successful international telepsychiatry programs. The support of international bodies and organizations are also integral in the development for guidelines, governance and policies to manage these programs (Wootton, 2003).
Application of telepsychiatry in Australia
Observational and benefit studies (Trott, 1998, Buist et al, 2000, Mielonen et al, 2000) highlight the cost benefit as well as patient and clinician acceptance of telepsychiatry practices in Australia. From the studies it is clear that although the initial establishment costs are high and therefore no significant savings are justified in the initial years of service, the cost savings thereafter for the patients were significant.
Telepsychiatry is proving successful through a number of programs to service rural Australian regions (such as wagga wagga, Dubbo, Western Australia and South Australia) across different psychiatric services.
Mental health is currently a significant user of real-time communication services across all Australian states (Buist, 2002, Suler, 2002, Parsons et al, 2002). In Australia, telepsychiatry has allowed psychiatry and psychology trainees to access supervision through videoconferencing allowing them to take advantage of the experience of rural psychiatry while continuing to receive supervision (Buist, 2002). The services delivered, the benefits of cost savings associated with the travel, accommodation, clinician availability and the improvement of quality life of the patients are all critical factors contributing to the success of telepsychiatry in Australia. Telepsychiatry and e-mental health are certainly here to stay (Wootton, 2003). Australia has been internationally recognized as a leader in the introduction and trial of telepsychiatry (RANCP, 2002). The driver for this has been the need and demand of psychiatry in Australian rural areas. The current challenges for telepsychiatry in Australia all relate to the human aspects of accepting the changes telepsychiatry impose on current conventional practice rather than lack of technology or lack of expertise associated with these practices.
Barriers and Limitations
Lack of Guidelines
The purpose of any medical guideline is to improve the effectiveness and efficiency of clinical practice, provide better clinical outcomes and enhance the reliability of medical services (Wootton, 2003). From a legal view, these guidelines offer a form of immunity to the health care professional (Stanberry, 1999). Formal telepsychiatry guidelines and policies are internationally scarce. The lack of these guidelines can be a logical explanation to the reluctance and resilience of implementing telepsychiatry. The lack of guidelines also suggests that there are certain obstacles to their development (Wootton, 2003). These obstacles are socially referred to as “bureaucracy”. Policy issues associated with telepsychiatry such as duty of care, medical indemnity and the need for registration across state boundaries are all unclear issues with no universal guidelines developed to clarify these issues. Two studies clearly illustrated the need for the development of universal guidelines to govern telepsychiatry practices. The first example is a pilot project conducted in Denmark (Mucic, 2007) to provide psychiatric services to immigrants/refugees in their own language. This project was established in order to address the great shortage of psychiatrists in the country in particular those serving the large immigration/refugee population, which makes up 8.2 % of the country’s population (Udlaendingestyrelsen, 2004). Although results of this study indicated positive response from the patients, participant clinicians expressed reluctance and opposition towards the program, preferring the services of translators. The introduction of an alternative means of treatment for this population base via telepsychiatry with professionals from other countries poses a number of threats and concerns not just for Danish psychiatrists, but also for the quality of care provided to the patients. These threats included: accountability for care, consistency in the provision of care in accordance with the countries’ medical policies and guidelines as well as the costs associated with treatment. A community telepsychiatry program in Kansas (Doolittle, 2001) is another example whereby a projected and extensive approach to applying telepsychiatry lacked structure, coordination and organization. This resulted in a loss to return on investment and minimal utilization of established services. The program plan was to facilitate access to care for rural psychiatric clients by using telemedicine to share clinical staff (i.e. for special expertise or cross-coverage) between mental health facilities. The telepsychiatry service was to include new patient evaluations, post-hospitalization follow up, and coordination of treatment and second opinions. Funding for the project came from state sources and totaled over $500,000. The loose organization of the community mental health centers proved not to be adequate to coordinate and implement this service. Sharing resources and cross-coverage also proved to be difficult between the health centers. Equipment for this program was purchased however remained idle and not used (Doolittle, 2001). Development of policies and guidelines to govern telepsychiatry practices are crucial to the success of these services.
Legal and ethical implications - Issues associated with privacy, security and confidentiality.
Privacy, security and confidentiality are all ethical and legal aspects presenting many implications of concern to therapists as well as patients participating in telepsychiatry. The legal and ethical implications in telepsychiatry are critical factors requiring clarity and awareness for the benefit of the patients and clinicians.
In Australia, the mental health Act was modified in 2002 for two states (QLD and Victoria) to mention the use of videoconferencing as a medium by which psychiatrists may perform legal assessment (Wootton et al, 2003).
Although a distinct advantage of using online telepsychiatry is the anonymity and confidentiality of the patient, this presents many ethical and legal challenges in emergency situations. Psychologists have an ethical duty to warn or duty to protect if clients present a danger to themselves or others (APA Ethics Code 4.05b3). Counseling psychologists are able to intervene in the case of an emergency only if they have information (Mallen et al, 2005) “One of counseling psychologists’ primary ethical responsibilities in practicing therapy is to avoid harming the client” (APA Ethics Code 3.04). Another ethical and legal challenge (primarily for online counseling) is the proof of licensing in the state or country of treatment and also accreditation of the therapist “(Mallen et al. 2005). The pilot project in Denmark reviewed in this study (Mucic, 2007) is an example demonstrating the potential for a broader need of international licensing and accreditation of therapists if they are to treat patients in different international locations. The ability to store and save records of counseling sessions poses many ethical and legal concerns. These ethical and legal issues demonstrate the need for therapists and also users to be aware when using telepsychiatry services.
Lack of economic studies
In order to effectively analyze the cost and consequences, it is beneficial to compare the costs of a conventional/traditional psychiatry service against the cost of a telepsychiatry service.
The table below compares the costs for both traditional psychiatry and telepsychiatry (via videoconferencing) from one study reviewed (Harley, 2006).
| Component | Videoconferencing | Traditional Method |
| Fixed costs | ||
| Videoconferencing unit: monitor, camera and ISDN installation_ per year | 5874.00 | - |
| Telecommunication line rental per year | 933.72 | - |
| Total fixed cost | 6807.72 | - |
| Variable costs | ||
| ISDN call charges | 158.40 | - |
| Travel and transfer | 21,000.00 | |
| Escort based on two registered nurses | 1950.00 | |
| Subsistence include meals and hotel stay | 3000.00 | |
| Total variable cost | 158.40 | 25,950.00 |
| Total costs | 6966.12 | 25,950.00 |
Table 3 Estimated annual costs (£) for using videoconferencing and traditional methods, based on 22 telepsychiatry episodes (10 Patient consultations and 12 specialist presentations)
The following is a graph of the total costs of the services for traditional methods versus telepsychiatry
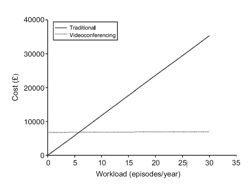
Figure 1 Total cost of providing telepsychiatry services (patient consultations and specialist presentations) by traditional means and by videoconferencing at different workloads (Harley, 2006)
It can be clearly seen from this table and the graph that the initial costs of telepsychiatry compared to traditional practice are high, however once a service is established there is a clear economic advantages in the use of telepsychiatry.
In another feasibility study conducted by Werner and Anderson (Werner, 1998), in a rural county in Michigan, the analysis required the inclusion of a wide range of cost elements including: equipment, clinic personnel, installation, maintenance, training, duplication of files, office space and line rental. These are all analysis elements required to be investigated in any cost-benefit analysis and cost evaluation of telepsychiatry.
Krupenski et al (Krupenski, 2002) also provides an example in Arizona of the long term cost barriers that can be confronted with telepsychiatry implementations. Patients missing, not attending or canceling appointments are considered normal activities, which need to be accounted for as part of the sustainability and durability of such programs.
Economically, telepsychiatry would be beneficial from both the patient and psychiatrists view in relation to cost savings due to the convenience of the service. However these are not the only stakeholders involved in this practice. Health directors and policy makers also play a pivotal role in establishing the policies and guidelines surrounding mental health practice. More evaluation and cost benefit literature studies are required in order to justify the economic benefit of telepsychiatry.
Conclusion
The potential for telepsychiatry services to assist in the provision of effective mental and psychiatric health care is constantly evident and increasing. The current forms of communication technologies (both synchronous and asynchronous) are proving to be adequate in use and these technologies are continually being enhanced for the benefit of practices. The need for further evaluations and application of these technologies to wider communities such as developing countries would ensure the accessibility of services to a wider range of the world’s population.
References
1. Alberta Heritage Foundation for Medical Research HTA 34 Health Technology Assessment
http://www.ahfmr.ab.ca/download.php/b16fcd38bc0f1677521414dc31d7e802
(last searched 12 June 2006)
2. American Psychological Association, (1997). “APA statement on services by telephone,teleconferencing, and Internet”. Retrieved March 8, 2004, from http://www.apa.org/ethics/stmnt01.html
3. American Psychological Association, (2002). “Ethical principles of psychologists and code of conduct”. Washington, DC: Author.
4. American Psychological Association. (2003). “Multicultural guidelines on education and training, research, practice and organizational development for psychologists”. American Psychologist, 58, 377.
5. Austen, S, Mcgrath, M, (2006) “Attitudes to the use of videoconferencing in general and specialist psychiatric services”, Journal of Telemedicine and Telecare Volume 12 Number 3
6. Barak, A (2007) “Emotional support and suicide prevention through the Internet: A field project report”, Computers in Human Behaviour Volume 23, Issue 2, Pages 971-984
7. Barker, D (2003), “Tele-Mental Health: An Examination of Use In Military Geographically Separated Units”, Bowie State University Maryland in Europe
8. Boydell, KM, Greenberg, N, Volpe, T (2004), “Designing a framework for the evaluation of paediatric telepsychiatry: a participatory approach”, Journal of Telemedicine and Telecare 10: 165–169
9. Braithwaite, D. O.,Waldron, V. R., & Finn, J. (1999). “Communication of social support in computer-mediated groups for people with disabilities.” Health Communication, 11, 123-151.
10. Buist A, Coman C, Silvas, A, Burrows G (2000) “An evaluation of the telepsychiatry programme in Victoria, Australia”, Journal of Telemedicine and Telecare Volume 6 Number 4
11. Buist A, (2002) “Telepsychiatry in Australia” in book “Telepsychiatry and e-Mental Health”, Royal Society of Medicine Press Ltd.
12. Chen DT, Blank, MB, Worrall, BB (1999) “Defending Telepsychiatry”, PSYCHIATRIC SERVICES © February Vol. 50 No. 2
13. De Las Cuevas, Arredondo, MT, Cabrera MF, Sulzenbacher H, Meise, U (2006) “Randomized Clinical Trial of Telepsychiatry through videoconference versus Face-to-Face Conventional Psychiatric Treatment”, Telemedicine and e-Health Volume 12, Number 3
14. De Las Cuevas L, Artiles J, De La Fuente J, Serrano, P (2003), “Telepsychiatry in the Canary Islands: user acceptance and satisfaction”. Journal of Telemedicine and Telecare 9: 221–224
15. Doolittle, GC (2001) “Telemedicine in Kansas: the successes and the challenges”, Journal of Telemedicine and Telecare 2001; 7 (Suppl. 2): S2:43–46
16. Doze S, Simpson, J., Hailey, D, et al (1999), “Evaluation of a telpsychiatry pilot project”, Journal of Telemedicine and Telecare, 5, 38-46
17. Farallel, SP, McKinnon CR (2003), “Technology and Rural Mental Health”, Archives of Psychiatric Nursing, Vol. XVII, No. 1 pp 20-26
18. Feinichel, M et al (2001), “Myths and Realities of Online Clinical Work”, A 3rd-Year Report from ISMHO's Clinical Case Study Group, 2001 APA Convention Presentations
19. Freuh B et al, (2000), “Procedural and Methodological Issues in Telepsychiatry Research and Program Development”, Psychiatric Services Vol. 51 No. 12
20. Freuh B et al, (2008), “Therapist Adherence and Competence With Manualized
Cognitive-Behavioral Therapy for PTSD Delivered via Videoconferencing Technology”, Behav Modif ; 31; 856
21. Greenwood J, Chamberlain C, Parker G (2004), “Evaluation of a rural telepsychiatry service”
Australasian Psychiatry Vol 12, No 3
22. Godleski, L (2004), “Telemental Health - The New Era”, Conference Presentation, International Telehealth Conference, March 4-5, Anchorage, Alaska
23. Grubaugh, AL, et al (2008) “Attitudes Toward Medical and Mental Health Care Delivered Via Telehealth Applications Among Rural and Urban Primary Care Patients”, Journal of Nervous & Mental Disease. 196(2):166-170
24. Hailey D, Jacobs P (1997) “Assessment of telehealth applications”, Alberta Heritage Foundation for Medical Research, Alberta, Canada.
25. Hailey, D., Bugler, T., Stayberg, S., et al. (2002). “The evolution of a successful telemedicine mental health service”, J Telemed Telecare, 8 Suppl 3, 24- 26.
26. Hailey, D., Roine, R., Ohinmaa, A. (2002). "Systematic review of evidence for the benefits of telemedicine" J Telemed Telecare 8 (Suppl. 1): S1. 1-30
27. Hailey,D., Ohinmaa,A., Roine,R., (2003). “Recent studies in assessment of telemedicine: systematic review of study quality and evidence of benefit”. Institute of Health Economics, Canada, Working Paper Number 2003-04.
http://www.ihe.ca./publications/papers/pdf/2003-04paper.pdf.
Last searched 16 October 2007
28. Hailey D, Ohinmaa A, Roine R. (2004) “Evidence for the benefits of telecardiology applications”: a systematic review (1992 to September 2003)
29. Hawthorne L, Birrell B (2002), “Doctor Shortages and their impact on the quality of medical care in Australia, People and Place”, vol 10, no 3, pp55-67
30. Håkansson S, Gavelin, C (2000), “What do we really know about the cost effectiveness of telemedicine?”, Journal of Telemedicine and Telecare Volume 6 Supplement 1
31. Harley J (2006), “Economic evaluation of a tertiary telepsychiatry service to an island”, Journal of Telemedicine and Telecare 2006; 12: 354–357
32. Harrison R, MacFarlane A, Wallace P (2002), “Implementation of telemedicine: the problem of evaluation”, Journal of Telemedicine and Telecare; 8 (Suppl. 2): S2:39 40
33. Hilty DM, Liu W, Marks S, Callahan EJ (2003) “Telepsychiatry: The Effective ness of Telepsychiatry: A Review”, CPA Bul le tin de l’APC—october
34. Hilty DM, Liu W, Marks S, Urness D, Yellowlees PM, Nesbitt TS (2004) “Clinical and Educational Telepsychiatry Applications: A Review”, Can J Psychiatry, Vol 49, No 1, January 2004
35. Hogenbirk, JC, Montgomery P, Boydell, KM, Pong RW, MA, DC (2006) “Using Telehealth to Augment Delivery of Mental Health Services by Family Health Teams: Potential Barriers and Possible Solutions”, Centre for Rural and Northern Health Research
36. Houston, T. K., Cooper, L. A., & Ford, D. E. (2002). “Internet support groups for depression: A 1-year prospective cohort study”. American Journal of Psychiatry, 159, 2062-2068.
37. Hyler, SE, Gangure, PD (2003), “A Review of the Costs of Telepsychiatry”, Psychiatric Services Vol. 54 No. 7
38. Johnsen, J.-A. K., Rosenvinge, J. H. & Gammon, D. (2002). “Online group interaction and mental health: An analysis of three online discussion forums”, Scandinavian Journal of Psychology,43, 445–449.
39. Jones,NB (2001), “Telepsychiatry and Geriatric Care”, Current Psychiatry Reports, 3:29–36
40. Kennedy, C, Yellowless, P (2000), “A community-based approach to evaluation of health outcomes and costs for telepsychiatry in a rural population: preliminary results”, Journal of Telemedicine and Telecare Volume 6
41. Kids Help Line, (2006), “Kids Help Line, 1800 551 1800”, Mass Media Studio,
Australia, Retrieved May,19, 2007 from http://www.kidshelp.com.au.
42. Kroll, T, Barbour R, Harris J (2007) “Using Focus Groups in Disability Research”, Qualitative Health Research, Vol. 17, No. 5, 690-698
43. Krupinski, E, et al (2002), “Chapter 2 : Clinical Applications in Telemedicine/Telehealth”, Telemedicine Journal And e-Health
Volume 8, Number 1, 2002
44. Laugharne, J, Janca, A. (2007), “ICD-10 telepsychiatry education in Western Australia: bridging the distance”, Primary Care And Community Psychiatry VOL. 12, NOS. 3–4, DECEMBER, 145–149
45. Leonard, S (2004), “The development and evaluation of a telepsychiatry service for prisoners”, Journal of Psychiatric and Mental Health Nursing, 11, 461–468
46. Majumdar, A.K (2007) “Advances In Telemedicine And Its Usage In India”, 15th International Conference on Advanced Computing and Communications, IEEE
47. Mallen, JM, Vogel DL, Rochlen, AB (2005), “The Practical Aspects of Online Counseling: Ethics, Training, Technology, and Competency”, The Counseling Psychologist, Vol. 33 No. 6.
48. Mallen, JM, Vogel, DL, Rochlen, AB, Day, SX (2005), “Online Counseling: Reviewing the Literature From a Counseling Psychology Framework”, The Counseling Psychologist, Vol. 33 No. 6, November 819-871
49. Maritz, J, Holroyd, S (2006), “Characteristics of Telephone Calls in a Psychiatric Outpatient Practice.”, Journal of Psychiatric Practice.12(3):195-199
50. Mattarelli, E , Weisband S (2006) “Exploring Telemedicine Success Over Time: A Case Study of the Arizona Telemedicine Program”, Organizational Communication and Information Systems (OCIS) division of the Academy of Management, Atlanta, Georgia
51. Mcginty KL, Simmons, SC (2006) “Telepsychiatry and e-Mental Health Services: Potential for Improving Access to Mental Health Care”, Psychiatry Q (2006) 77:335–342
52. Meier A, Lyons EJ, Frydman G, Forlenza M, Rimer, BK (2007), “How Cancer Survivors Provide Support on Cancer-Related Internet Mailing Lists”, J Med Internet Res. 9(2): e12
53. Merkel, L (2004) “RURAL MENTAL HEALTH”, Research Paper
54. Mielonen ML, Ohinmaa A, Morin J, Isohanni M.(2000), “Psychiatric inpatient care planning via telemedicine”, Journal of Telemedicine and Telecare;6:152
55. Miller, JK, Gergen, KJ. (1998), “Life on the Line: The Therapeutic Potentials of Computer-Mediated Conversation”, Journal of Marital and Family Therapy, v24 n2 p189-202
56. Miller, EA, (2002), “Telemedicine and doctor-patient communication: a theoretical framework for evaluation”, Journal of Telemedicine and Telecare;8:313-318
57. Mitchell et al (2008), “A randomized trial comparing the efficacy of cognitive–behavioral therapy for bulimia nervosa delivered via telemedicine versus face-to-face”, Behaviour Research and Therapy 46, 581–592
58. Modai, I, Jabarin, M, Kurs, R, Barak P, Hanan, I, Kitain L (2006) “Cost Effectiveness, Safety, and Satisfaction with Video Telepsychiatry versus Face-to-Face Care in Ambulatory Settings”, TELEMEDICINE AND e-HEALTH Volume 12, Number 5
59. Monnier J, Knapp R, Frueh, BC (2003) “Recent Advances in Telepsychiatry:
An Updated Review”, PSYCHIATRIC SERVICES Vol. 54 No. 12
60. Mucic, D (2007) “Telepsychiatry pilot-project in Denmark Videoconference by distance by ethnic specialists to immigrants/refugees”, WCPRR 3-9
61. Myers, K, Valentine MJ, Melzer SM (2007) “Feasibility, Acceptability, and Sustainability of Telepsychiatry for Children and Adolescents”, PSYCHIATRIC SERVICES Vol. 58 No. 11
62. Myers, KM, Valentine MJ, Melzer, SM (2008) “Child and Adolescent Telepsychiatry: Utilization And Satisfaction”, MARY ANN LIEBERT, INC. VOL. 14 NO. 2
63. Newman, MJ, (2004), “Technology in Psychotherapy: An Introduction”, JCLP/In Session, Vol. 60(2), 141–145
64. NHS Direct Foundation Trust (2008), http://www.nhsdirect.nhs.uk/articles/article.aspx?articleId=302 (last searched 02 June 2008)
65. Norman, S (2006), “The use of telemedicine in psychiatry”, Journal of Psychiatric and Mental Health Nursing, 13, 771–777
66. O’Reilly R, Bishop J, Madox K et al (2007) “Is Telepsychiatry Equivalent to Face-to-Face Psychiatry? Results From a Randomized Controlled Equivalence Trial”, PSYCHIATRIC SERVICES Vol. 58 No. 6
67. Parsons J, Merlin T, Taylor J, Wilkinson D, Hiller J (2002) “Evidence-basedpractice in a ruraland remote setting A critical literature review”, Health Technology Assessment Unit, Department Of Public Health, University Of Adealaide
68. Pesa¨maa, L, Ebeling, H, Kuusima¨ki M, Winblad I, Isohanni, M, Moilanen I (2004) “Videoconferencing in child and adolescent telepsychiatry: a systematic review of the literature”, Journal of Telemedicine and Telecare 10: 187–192
69. Pott, H (2005), “Online support groups: An overlooked resource for patients”, Chime article.
70. Rahman, A (2006), “E-Mental health in Pakistan: a pilot study of training and supervision in child psychiatry using the internet”, Psychiatric Bulletin 30: 149-152
71. Royal Australian and New Zealand College Of Psychiatrists (2002) “TELEPSYCHIATRY”, Position Statement #44
72. Simpson, J., Doze, S., Urness, D., et al. (2001) “Evaluation of a routine telepsychiatry service”, J Telemed Telecare, 7, 90-98.
73. Simpson, J., Doze, S., Urness, D., et al. (2001) “Telepsychiatry as a routine service - perspective of the patient”, J Telemed Telecare, 7, 155-160.
74. Smith HA, Allison RA (1998) “TELEMENTAL HEALTH: Delivering Mental Health Care at a Distance”, U.S. Department Of Health And Human Services, Rockville, MD
75. Stanberry, B. (1999), “Meicolegal aspects of telemedicine”. In: Wootton, R, Craig J, Introduction to Telemedicine, London, Royal Society of Medicine Press, 1999: 159-175
76. Starling J, Rosina R, Nunn, K Dossetor, D (2003) “Child and adolescent
telepsychiatry in New South Wales: moving beyond clinical Consultation”, Australasian Psychiatry Vol 11 Supplement
77. Starling J, Foley S (2006), “From Pilot to Permanent Service: ten years of paediatric telepsychiatry”, Journal of Telemedicine and Telecare, Volume 12, Supplement 3, pp. 80-82(3)
78. Suler, J (2002). “The online clinical case study group: An e-mail model, Cyberpsychology and Behavior”, Dec 4(6), pp. 711-22
79. Tate, D, Zabiniski, M (2004), “Computer and Internet Applications for Psychological Treatment: Update for Clinicians, JCLP/In Session, Vol. 60(2), 209–220”
80. Tate DF, Jackvony EH, & Wing RR, (2003); “Effects of Internet Behavioral Counseling on Weight Loss in Adults at Risk for Type 2 Diabetes”, JAMA. 2003;289:1833-1836
81. Tate DF, Wing RR, & Winett RA, (2001), “Using Internet Technology to Deliver a Behavioral Weight Loss Program”, JAMA. 2001;285:1172-1177.
82. Trott P, Blignault I (1998), “Cost evaluation of a telepsychiatry service in northern Queensland”. Journal of Telemedicine and Telecare; 4(suppl. 1):66-8
83. Udlændingestyrelsen. Nøgletal på udlændingeområdet, 2004
84. Umess, D (2003) “Telepsychiatry and Doctor–Patient Communication: A Tale of Two Interviews”, CPA Bulletin de l’APC—October
85. VandenBos GR, Williams S. (2000). “The Internet versus the telephone: What is telehealth, anyway?” Professional Psychology: Research and Practice, 31, 490-492.
86. Vassallo D J, Hoque F, Farquharson RM, Patterson V, Swinfen P, Swinfen R (2001), “An evaluation of the first year's experience with a low-cost telemedicine link in Bangladesh”, Journal of Telemedicine and Telecare, Volume 7, Number 3, pp. 125-138(14)
87. Wagnild, G, Leenknecht C, Zauher J (2006) “Psychiatrists’ Satisfaction with Telepsychiatry”, Telemedicine And e-HEALTH Volume 12, Number 5
88. Walstrom, MK (2000), “You Know, who’s the Thinnest?: Combatting surveillance and creating safety in coping with eating disorders online, CyberPsychology and Behavior, 3, 2000, pp.761-783.
89. Werner A, Anderson LE, (1998), “Rural Telepsychiatry is economically unsupportable, the Concorde crashes in a cornfield”, Psychiatric services, 49; 1287-1290
90. Whitten, P, Zaylor C, Kingsley C (2000) “An Analysis of Telepsychiatry Programs from an Organizational Perspective”, Cyberpsychology & Behavior Volume 3, Number 6
91. Whitten, P, Rowe-Adjibogoun, J (2002) “Success and failure in a Michigan
telepsychiatry programme”, Journal of Telemedicine and Telecare 8 (Suppl. 3): S3:75 77
92. Wootton, R, Yellowlees, P, Mclaren, P (2003), “Telepsychiatry and e-Mental Health”, Royal Society of Medicine Press Ltd.
93. Wootton, R., Craig, J.& Patterson V. (2nd Edition.) (2006). “Introduction to Telemedicine”. London: Royal Society of Medicine Press.
94. Yellowlees P (2001) “An analysis of why telehealth systems in Australia have not always succeeded”, Journal of Telemedicine and Telecare; 7 (Suppl. 2): S2:29–31
95. Yellowlees PM, Kennedy C.(1997) “Telemedicine: here to stay”. Medical Journal of Australia;166:262-5
96. Yellowlees P (2000) “The future of Australasian psychiatrists: online or out of touch?”, Australian and New Zealand Journal of Psychiatry 34:553–559
97. Zaylor C, Nelson EL, Cook DJ (2001): “Clinical outcomes in a prison telepsychiatry clinic. Journal of Telemedicine and Telecare 7(suppl 1):47–49, 2001
First Published October 2009
Copyright Priory Lodge Education Ltd. 209
Click
on these links to visit our Journals:
Psychiatry
On-Line
Dentistry On-Line | Vet
On-Line | Chest Medicine
On-Line
GP
On-Line | Pharmacy
On-Line | Anaesthesia
On-Line | Medicine
On-Line
Family Medical
Practice On-Line
Home • Journals • Search • Rules for Authors • Submit a Paper • Sponsor us
All pages in this site copyright ©Priory Lodge Education Ltd 1994-


