Browse through our Journals...
A Complicated Case of Herpes Simplex Encephalitis
Herpes Simplex Encephalitis Complicated By Cerebral Venous Sinus Thrombosis and Dental Trauma
Ewan Hunter, Fiona McGill, Edmund Ong. Department of Infectious Diseases, Newcastle General Hospital.
Presentation and diagnosis
A forty-seven year old gentleman who worked as an electrical engineer and part-time milkman presented to our acute admissions unit with a history of acute onset dizziness associated with fever and nausea, followed by seven days of headache, joint pains and general malaise. On the morning of admission his wife had noticed that he was confused, unsteady on his feet and having difficulty finding words. There was no past medical history of note, he was not taking any regular medication, and he drank alcohol only rarely.
On admission he was afebrile and haemodynamically stable, although it was noted that he appeared clinically dehydrated. On examination he was overtly confused, scoring 2 out of 10 on an abbreviated mental test score, and was found to be hyperreflexic throughout, with clonus in the lower limbs. Neurological examination was otherwise unremarkable, with intact cranial nerves, normal power and sensation and downgoing plantars. Cardiovascular and gastrointestinal examinations revealed no abnormalities.
Initial blood tests revealed a normal total white cell with a mild lymphopaenia of 0.9 x 109/L (lab reference range 1.5 – 4.0), a CRP of less than 5 mg/L (0-5) and an ESR of 20. Urea was 9.3 mmol/L (3.1 – 7.9), creatinine 95 µmol/L (70 – 110), and liver function was normal. A CT head was reported as normal. Lumbar puncture was subsequently performed, yielding cloudy CSF with an opening pressure of 40cm, a white cell count of 590/mm3 (90% lymphocytes), protein of 1.49 g/L (0 – 0.40), glucose 2.2 mmol/L (plasma 6.1), and no organisms seen on Gram stain. Samples were also sent for herpes simplex and enterovirus PCR. A presumptive diagnosis of viral encephalitis was made, and the patient was commenced on iv acyclovir at 10mg/kg TDS immediately following lumbar puncture.
Progress
By the following morning the patient was more alert and oriented, although renal function had deteriorated with a urea and creatinine of 10.3 and 129. Later that same day the patient was witnessed to have a tonic-clonic seizure, terminating spontaneously after less than a minute. He was commenced on phenytoin, and continued to improve over the next two days, with no further seizures. By day three he was feeling much better, although complained of jaw pain, and it was noted that his jaw was not closing properly. His co-ordination was also still mildly impaired with bilateral arm drift on examination. OPG images of the jaw were obtained immediately and MRI of the brain was requested. The first of these demonstrated bilateral fracture dislocations of the mandibles (image 1). He was reviewed by the maxillo-facial team, who recommended the insertion of arch bars. Shortly after, however, the MRI scan revealed extensive venous sinus thrombosis with bilateral parietal venous infarctions. Temporal lobes were normal (image 2). At the same time, PCR on the CSF was reported as positive for HSV-1. It was felt that the thrombus was most likely secondary to a prolonged dehydrating prodromal illness, and conservative management was advised, with follow-up imaging at three weeks and three months. The patient subsequently went to theatre for fixation of the mandible.
The patient’s neurological findings persisted, and by day ten of the admission he was experiencing dysaesthaesia of the left arm, and examination revealed a left sided sensory inattention and homonymous hemianopia. There was also weakness of finger abduction and wrist extension associated with pyramidal drift on the left and abnormal coordination. By the following morning these symptoms had largely resolved.
The patient completed 14 days of intravenous acyclovir and was discharged with follow-up under maxillo-facial surgery and infectious diseases. He was commenced on aspirin as an out-patient, and MRI at six months showed that the thrombosis had fully recanalised. There were no residual neurological deficits and his memory was intact. By way of an anecdotal measure of this, he was able to spontaneously recall the details of around three hundred individual orders on his milk round.

Image 1 – OPG demonstrating bilateral fracture dislocations of the mandible
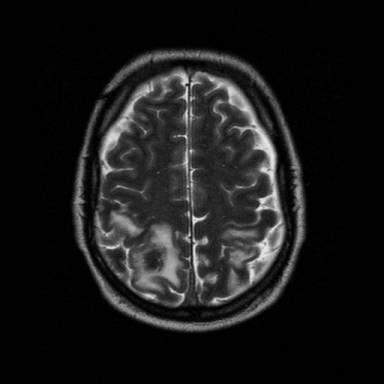
Image 2 – MRI demonstrating sinus thrombosis with parietal venous infarction
Discussion
Whilst enterovirus is the most common cause of viral encephalitis in the developed world, herpes simplex virus (HSV) is thought to be the most common cause of sporadic fatal encephalitis. HSV type I accounts for about 10% of all cases of encephalitis in the US, and has a bimodal age distribution, with most cases occurring in patients under 20 and over 50 years of age (Whitley RJ 1990, Whitley RJ, Gnann JW 2002). Over 70% of untreated patients will die, and even with treatment, mortality may reach 30% at one year, with only 2.5% of surviving patients making a complete neurological recovery (Whitley RJ, Roizman B 2001) . Both mortality and later sequelae can be reduced if therapy is instituted before there is a major alteration in consciousness (Whitley RJ e.a. 1986). The classical presentation of acute viral encephalitis is the triad of fever, headache, and altered level of consciousness, with additional clinical findings including disorientation, behavioural disturbance and focal or diffuse neurological abnormalities including seizures. CSF examination tends to reveal a mononuclear pleocytosis, an elevated protein level, and a normal or slightly low glucose.
Cerebral venous and sinus thrombosis (CVST) accounts for less than 1% of all strokes, with the exact incidence being unknown due to a lack of population-based studies (Masuhr F e.a. 2004). Headache is the most commonly reported symptom, occurring in up to 95% of all cases. Focal neurological signs are the most common findings, although a clinical picture of subacute encephalopathy with altered confusion, seizures or alterations in consciousness can be a misleading presentation (Bousser MG 2000). Typical CSF findings include a raised pressure and elevated protein count, with a mild lymphocytic or mixed pleocytosis (Masuhr F e.a. 2004). Underlying conditions predisposing to CVST are similar to those causing venous thrombosis in other parts of the body, although the aetiology remains unknown in up to 35% of cases (Bousser MG 2000). Treatment consists of anticoagulation to reduce sequelae and mortality.
Whilst CVST is often quoted as a differential diagnosis in cases of HSV encephalitis, we could find no formal reports in the literature of CVST being diagnosed in association with HSV encephalitis.
Seizure-related injury is a well documented problem. One tertiary epilepsy centre reported post-seizure orthopaedic injuries in up 5% of patients (Tiamkao S 2006), and an increased predilection to anterior dental injury has been observed in a Nigerian cohort of epilepsy patients (Ogundbedede e.a. 1998). Such injuries are largely due to falls, however, and we could find no specific reports of a mandibular fracture dislocation following a seizure.
Conclusion
This was a potentially misleading presentation, with a raised opening pressure on lumbar puncture, cloudy CSF and a markedly elevated protein count. While this may have been a clue to the presence of CVST as a complication, the prompt initiation of antiviral therapy was nevertheless the correct course of action. This was borne out by subsequent PCR findings and the impressive recovery made by the patient. The case also serves as a reminder that while seizures are a relatively common event in hospital in-patients, serious traumatic sequelae are possible and should be sought.
References
Bousser MG (2000) Cerebral venous thrombosis: diagnosis and management. J Neurol 247:252-258
Masuhr F, Mehrain S, Einhaupl K. Cerebral venous and sinus thrombosis. J Neurol (2004) 251: 11-23
Ogundbodede e.a., Oral Dental Health Needs in Nigerian Patients with Epilepsy, Epilepsia, 39(6): 590-594, 1998
Tiamkao S, Seizure-related injury in an adult tertiary epilepsy clinic, Hong Kong Med J, 12(4): 260-263
Whitley RJ. Viral encephalitis. N Engl J Med 1990; 323: 242 – 50
Whitley RJ, Alford CA, Hirsch MS et al. Vidaribine versus acyclovir therapy in herpes simplex encephalitis. N Eng J Med 1986; 314: 144-9
Whitley RJ, Gnann JW. Viral encephalitis: familiar infections and emerging pathogens. Lancet 2002; 359:507-14
Whitley RJ, Roizman B. Herpes simplex virus infections. Lancet 2001: 357 (1513 – 1518)
First Published February 2008
Copyright PrioryLodge Education Limited 2008
Click
on these links to visit our Journals:
Psychiatry
On-Line
Dentistry On-Line | Vet
On-Line | Chest Medicine
On-Line
GP
On-Line | Pharmacy
On-Line | Anaesthesia
On-Line | Medicine
On-Line
Family Medical
Practice On-Line
Home • Journals • Search • Rules for Authors • Submit a Paper • Sponsor us
All pages in this site copyright ©Priory Lodge Education Ltd 1994-


