Browse through our Journals...
A shared baby: two GPs and one addiction consultant grow their own ‘shared care scheme’ for drug using patients
Dr Sanju George1, Sylvie Boulay2 Mary Ryan3, Ann McDermott4, Dr Paul Wallace5, Dr Shyam Saikia6.
1Consultant in Addiction Psychiatry, The Bridge Substance Misuse Service, Birmingham and Solihull Mental Health NHS Trust (BSMHT), 2Team manager at The Bridge Substance Misuse Service (BSMHT), 3Substance Misuse Nurse, The Bridge Substance Misuse Service (BSMHT), 4Substance Misuse Nurse, The Bridge Substance Misuse Service (BSMHT), 5GP at The Castle Practice, Kingshurst, 6GP at 196 Green Lane, Castle Bromwich.
Abstract
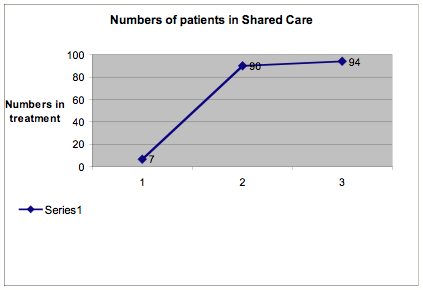
Shared care is the joint working of addiction specialists and GPs in treating drug - using patients. Its main objective is for stable drug users to be treated by their own GPs, which provides them with an opportunity to receive holistic care in a less stigmatising environment. Faced with difficulties in persuading most local (Solihull) GPs to treat their own drug using patients, the addiction consultant at the specialist drug service and two experienced GPs created an intermediate arrangement: the two GPs would provide a shared care service for all the other GPs’ patients with the support of the consultant and two dedicated substance misuse nurses. Flexible referral and re-uptake criteria and efficient joint working were key to success. The number of patients in shared care has gone up from 7 in May 2006 to 94 by November 2007. Patients are thrilled with the new system and more Solihull GPs are now prepared to take on prescribing for their own patients. This innovative shared care scheme has managed to overcome traditional boundaries to provide a seamless and user-friendly service to drug users. In this paper, we briefly describe how we went about setting up the scheme and some of the challenges we successfully overcame. We hope our model can offer some useful pointers for others. The scheme received national recognition when Dr Sanju George and his team were awarded the Hospital Doctor of the year Award for 2007 in the One Vision category (consultants and GPs working together).
Introduction
Shared care is defined as the joint working of addiction specialists and GPs in treating patients with drug misuse problems and it is a well-established and proven alternative to specialist treatment provision. The objective is for the more stable drug users to be treated by their own GPs: ‘GPs also have a role in the provision of care and treatment of drug misusers within a system of ‘shared care’ with a specialist drug service (Department of Health 1996). This is an opportunity for drug users to receive a more holistic treatment – not just substitute prescribing, but also a range of medical interventions, which can be provided in a GP setting. GPs already have in depth knowledge of their clients and are in a unique position to offer comprehensive treatment without any stigma. All drug users benefit because treating patients in shared care settings costs approximately half what it costs in specialist settings. The Department of Health’s latest version of the UK guidelines on clinical management for drug misuse and dependence (the ‘orange book) recognises how much primary care has moved on: ‘a single ‘shared care’ model – described in the 1999 Clinical Guidelines as partnerships between primary, secondary and specialist providers – has, in practice, developed into a range of different models, often driven by local circumstances and including a wider range of providers’. In this paper, we briefly describe how we went about setting up the scheme and some of the challenges we successfully overcame. We hope our model can offer some useful pointers for others.
The Setting
Solihull in 2005: a West Midlands Metropolitan Borough Council of around 200,000 residents, with one long established statutory (NHS) specialist service for Class A drug users (The Bridge) working closely with a voluntary drug service (Welcome) and a very small handful of GPs willing to take on the care of their drug using patients.
The problem
Given the above-noted benefits and the robust evidence base, the Solihull Drug Action Team (DAT) was very keen to have more patients in shared care in Solihull. With only 15 drug users in treatment with their own GPs, there was no hope of meeting the local target of 100 in shared care by the end of the year (2006). The best efforts of the consultant addiction psychiatrist – Dr Sanju George and the two substance misuse nurses at The Bridge had made little difference.
The solution: the birth of shared care in Solihull
The search for a solution led to the suggestion of an intermediate arrangement: if the majority of Solihull GPs were not ready to take on the care of their own drug using patients, then an option was to get two experienced GPs to provide a shared care service for all the other GPs’ patients. A local primary care setting, the Chelmsley Wood Primary care centre was chosen as the ideal setting. There was also a pharmacist on site willing to dispense methadone and buprenorphine (both substitute treatments for heroin addicts), and naltrexone. In June 2006, Dr Wallace and Mary Ryan, a very experienced substance misuse nurse at The Bridge, welcomed their first six patients at the Bosworth primary care centre, marking the birth of our shared care scheme.
Early development and challenges
Dr Wallace took on the lead developmental role and he was ably assisted by Dr Saikia and supported by the two substance misuse nurses.
There were many issues to be resolved to provide a service crossing the boundaries of two trusts - Birmingham and Solihull Mental Health NHS Trust (BSMHT) and the Solihull Care Trust. The practicalities included defining the support which would be provided by the specialist substance misuse clinicians, what arrangements would be made for patients who relapsed, how cover would be provided for the two GPs, how and where prescriptions would be produced, clinical governance issues and the thorny issue of where patients’ files would be kept.
The first step was to revise the previous strict criteria for patient eligibility for shared care. Dr George took the lead in revising the guidelines and introduced an unprecedented degree of flexibility. In the past only very stable drug users on methadone had been eligible. Under the new criteria agreed with the two GPs, drug users could also be offered buprenorphine or naltrexone. The previous exclusion relating to co-existing several mental illnesses was replaced with a criterion that the patient should currently be in treatment and relatively stable. A decision was made that all the criteria would be applied flexibly with joint decision-making by the doctors and substance misuse clinicians involved. The commitment was made by Dr George that patients who developed problems and needed to be referred back to the specialist service at The Bridge would be seen within five days at most.
The multi disciplinary team at The Bridge made a concerted effort to recruit as many patients as possible into the shared care scheme. In eighteen months the overall numbers in shared care has grown from 7 in May 2006 to 90 in July 2007 and 94 in November 2007. In the same period, 8 patients successfully completed their treatment and were discharged drug free.
How the team delivers first class patient care
Drug users are very satisfied with the scheme. Mr.A (anonymised) told Mary Ryan, his substance misuse clinician ‘It’s great to come to Bosworth, nobody knows why I’m here and I don’t bump into anybody I know’. Mr B is also full of praise for the new system. He was one of the first patients to move to the shared care scheme. He is now one of the user representatives and still returns to The Bridge regularly but only to take part in meetings with the consultant and his team. He says ‘there is no stigma attached to going to the doctor’s surgery; I got my teeth fixed by the dentist at the Bosworth primary care centre and I’d wanted to do that for years’.
The consultant and the two GPs discovered that a lot of preparation was needed for some long-term patients to transfer from the specialist clinic to the primary care centre. Three-way sessions were held with client and both specialist and shared care substance misuse clinicians to ease the transition and a new referral form was devised.
Inevitably some patients’ circumstances change, either because physical or mental health problems worsen or short term lapse turns into full relapse. In this case patients are transferred back into the care of the consultant at The Bridge within five days at the most. As soon as they become stable they can transfer back to the primary care centre.
The substance misuse nurses discuss in the weekly team meetings at The Bridge any shared care patients they are concerned about so that the consultant continues to be involved in the package of care and is ready to take over when needed. He is also constantly available on the phone for advice.
Shared Care for Drug Misusers in Solihull
Patient referred back to The Bridge if specialist treatment needed
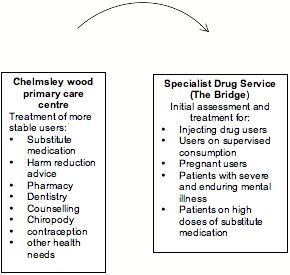

Patient referred to the primary care centre as soon as stable enough
How is our shared care scheme unique?
Our shared care scheme represents a unique bridging of the traditional barriers between secondary and primary care services: every member of the team is committed to making it work and the occasional problems are solved on the spot. If patients need urgent help on the days when the two GPs are not available, the consultant steps in. Likewise the two GPs are very flexible and will liaise with the two substance misuse clinicians on the days when they are not working in shared care. In addition the substance misuse nurses have regular supervision as a team.
The excellent links between the two services result in an outstanding continuity of care: drug users are able to become independent of the specialist service; they have the opportunity to manage a return to normality; for a significant proportion, this is the first time that they have been able to commit to training or new employment opportunities. At the same time they know the safety net of returning to The Bridge is always available if needed.
The three doctors and the two substance misuse clinicians work in a very flexible way. Although there are clear eligibility criteria for shared care, exceptions are frequently made: recently a pregnant patient with severe physical problems asked to stay in shared care and this was agreed with regular monitoring by all involved. If for any reason it is easier for a patient to see their substance misuse clinician at The Bridge rather than at the primary care centre, interviews are booked at The Bridge. Any group activity such as large-scale blood borne virus testing or vaccination takes place at The Bridge.
A great deal of development work takes place to persuade more Solihull GPs to take on their own patients and the consultant, the two GPs and the substance misuse clinicians share this by doing presentations, visiting medical colleagues etc… Patients also spread the word and gently encourage their own GPs to take part in the scheme.
User feedback
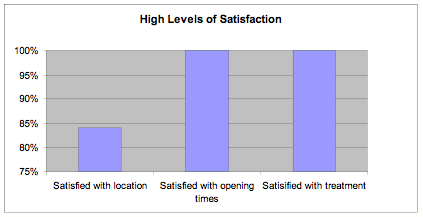
In order to identify the benefits of the scheme to users, we developed a simple and user-friendly questionnaire that was handed out to 40 patients in shared care in June 2007. The questionnaire consisted of questions on the location, opening times and satisfaction with treatment, which were to be rated on a scale of 1 to 10 (1 = not all satisfied and 10 = extremely satisfied). There was also space provided for comments and suggestions. The quantitative and qualitative results are given below.
We received 19 responses, i.e. a response rate of 48%. Our results showed that 84% of respondents rated convenience of location at 5 or above with 58% rating it at 8 or above. 68% of respondents rated convenience of opening times at 8 or above and no one rated it below 5. Satisfaction with treatment was very high – 84% rating it at 8 or above and no one rating it below 5.
Respondents were asked what they liked about the Chelmsley Wood Primary Care Centre: many people commented on privacy: ‘I like the fact that no one knows what I’m coming here for’. ‘It is more discreet for myself as I have to take my son with me’, ‘don’t bump into people’, ‘it’s more private so I can talk more openly with my own counsellor’. Many valued the different ‘look’ of the centre: ‘It feels less like a drug clinic’, ‘a friendly, quiet and clean place’, ‘not like going to a drug clinic and very clean and helpful’. Many respondents had made use of other facilities at Bosworth: 5 had used the dentist, 8 used the pharmacy, 1 the contraceptive clinic and 1 the counselling service. Interestingly three people volunteered that they saw their own GP at the centre. Respondents clearly liked being able to meet other needs there: ‘it’s friendly, caring and local and caters to all needs’, ‘I like the other services that are offered to me’,
Conclusion
The Solihull shared care scheme represents a unique approach with one specialist addiction consultant and two experienced GPs and their teams committed to overcome traditional boundaries to provide a seamless and user-friendly service to drug users. Thanks to our shared care scheme the drug system in Solihull goes a long way to meeting the key message of the Royal College of General Practitioners and the Royal College of Psychiatrists that ‘commissioners should ensure local treatment systems have a complete spectrum of medical provisions to meet the range of needs and the numbers of substance misusers entering treatment. This requires a variety of skills and competencies at various levels, from simply providing general medical skills, to GPs offering less complex drug treatments, to specialist addictions skills and addiction psychiatry skills’ (Department of Health 2006). We hope our model offers useful pointers for others.
References
Department of Health (1996), Task Force to Review Services for Substance Misusers: Report of an independent Review of Drug Treatment Services in England, London, HMSO.
Department of Health (July 2006), Models of Care for the treatment of adult drug misusers: update 2006, National Treatment Agency for Substance Misuse.
Department of Health (2007), Drug misuse and dependence, UK guidelines on clinical management, London.
Declaration of interest: None
Acknowledgements: We thank all users who participate din the survey.
First Published March 2008
Copyright Priory Lodge Education Limited 2008
Click
on these links to visit our Journals:
Psychiatry
On-Line
Dentistry On-Line | Vet
On-Line | Chest Medicine
On-Line
GP
On-Line | Pharmacy
On-Line | Anaesthesia
On-Line | Medicine
On-Line
Family Medical
Practice On-Line
Home • Journals • Search • Rules for Authors • Submit a Paper • Sponsor us
All pages in this site copyright ©Priory Lodge Education Ltd 1994-


