Browse through our Medical Journals...
Pleural Infections in the Intensive Therapy Unit
Vijayan, S K
“Pus Blonum Ectadabil” – “Wherever there is pus, drain it”, Hippocrates ~400BC.
Definitions
A pleural effusion is defined as excessive accumulation of fluid in the pleural space. Pleural effusions associated with pneumonia can be subdivided into simple (do not need drainage) or complicated (need drainage) parapneumonic effusions. An empyema is a collection of pus in the pleural cavity.
Frequency
- Common causes include Pneumonia (82%), Tumour (8%), Surgery (6%), TB (3%), Foreign body (1%)
- ~50,000/year admissions with pneumonia in UK
o Up to 40% develop pleural fluid of which 10% need drainage
- ITU : Patients frequently develop pleural effusions
Hypoalbuminaemia, atelectasis, heat failure common causes
Drainage may facilitate weaning
When to suspect a pleural collection
- Failure to respond to appropriate antibiotic treatment for pneumonia
- Unknown source of sepsis
Causes of pleural effusions:
Transudates Exudates
Common Causes
• Left ventricular failure
• Liver cirrhosis
• Hypoalbuminaemia
• Peritoneal dialysis
Less common causes
• Hypothyroidism
• Nephrotic syndrome
• Mitral stenosis
• Pulmonary embolism (10-20%)
Rare causes
• Constrictive pericarditis
• Meig’s syndrome
• Urinothorax
Common Causes
• Malignancy
• Parapneumonic effusions
• Tuberculosis
Less common causes
• Pulmonary embolus (with infarction)
• Rheumatoid arthritis
• Autoimmune diseases
• Benign asbestos effusion
• Pancreatitis
• Chylothorax
• Post-myocardial infarction
• Sarcoidosis
Rare causes
• Oesophageal perforation
• Yellow Nail Syndrome
• Drugs
Symptoms and Signs
- Variable according to the amount of pleural fluid present
- Pleuritic chest pain, dyspnoea, non productive cough, swinging pyrexia
- Physical findings include dullness on percussion, diminished breath sounds, reduced tactile fremitus
- ITU: Often difficult to assess due to patient positioning and chest wall oedema
Imaging
Chest radiography (CXR)
AP film:
- Usually obvious
- If pulmonary infiltrates and fluid present – suspect parapneumonic collection
- Classical signs on erect film are:
o Blunting of costo-phrenic angle
o Homogenous opacification with no air bronchogram and a meniscus with
the apex towards axilla.
Supine film (often done in ITU)
- Underestimates quantity of pleural fluid
- Free fluid will layer out posteriorly
- Hazy opacity of one hemithorax
- Loss of sharp silhouette of hemidiaphragm
Ultrasound
More accurate than plain CXR for estimating fluid volume and aiding aspiration
- Effusions appear as an echo free layer between the visceral and parietal pleurae.
- Demonstrates loculations and helps differentiate fluid from pleural thickening
- Request a formal ultrasound scan if any doubt
Computerized Tomography
- Useful in cases of diagnostic difficulty
- Request with contrast enhancement
- Differentiates pleural fluid from lung abscess
- May be used to differentiate between benign and malignant pleural thickening.
- Useful if drainage difficult to delineate size and position of loculated effusions
Diagnosis
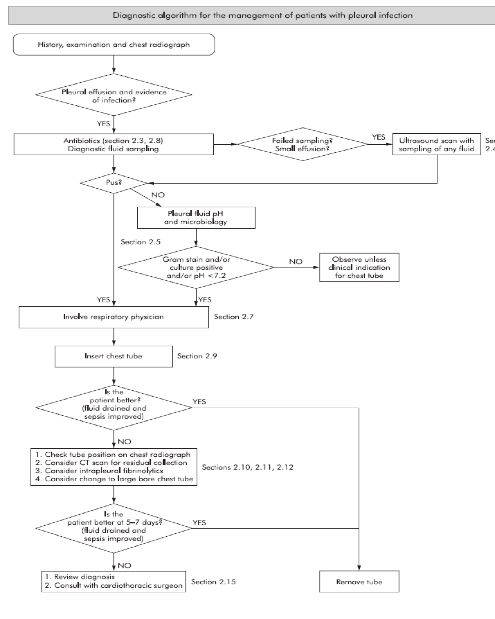
All patients with a pleural effusion & sepsis or pneumonia should have a DIAGNOSTIC PLEURAL ASPIRATION
Note the appearance and odour of any fluid
ITU: High frequency of other processes causing pleural effusion
If low infective risk and predisposing cause for effusion – observe
If features of sepsis present - Pleural aspiration + tube drainage
Laboratory Investigations
1. pH Place fluid in heparinised container and process on unit’s machine
Do not measure if frank pus (=empyema)
If pH <7.2 and effusion due to concurrent pneumonia – requires prompt chest tube insertion.
(Rheumatoid arthritis and malignancy may also cause low pH)
2. Protein Universal specimen bottle
Transudate <30g/l
If serum protein normal
Exudate >30g/l
Blood stained effusions are typically exudates
o If value 25 – 35 g/l, or serum protein abnormal:
• Light’s criteria will be performed
• This will be done automatically by biochemistry at Morriston
• Pleural fluid LDH will be measured as well as serum LDH and protein
• The biochemistry laboratory will provide an automated result
N.B. Light’s criteria may label some patients who actually have transudative effusions as exudates. This particularly occurs in patients who have received diuretics prior to thoracocentesis.
3. Glucose Grey bottle
Pleural fluid glucose low in empyema
Also low in Rheumatoid arthritis,Tuberculosis, SLE, malignancy.
4. Microbiology tests
o Culture (blood culture bottles) & AFB (white top bottle)
o Phone and request urgent Gram stain
5. Cytology
o If malignancy suspected clinically – white top bottle
Additional biochemistry tests (if indicated)
• Amylase High pleural concentrations (>200U dl-1) occurs in both acute
and chronic pancreatitis, malignancy and oesophageal rupture.
• Triglycerides and Cholesterol
• Chylothorax - high triglycerides, low cholesterol
• Psuedochylothorax - high cholesterol, low triglycerides
Management
1. What antibiotics should be given?
• All patients should receive antibiotics – for 3 weeks in total.
• Where possible, be guided by bacterial culture results.
• Initial antibiotic choice reflects the organisms likely to be responsible.
• If patient has cultured organism in sputum/blood culture previously – adapt antibiotic prescription to reflect this.
• If result of Gram stain available – adapt antibiotic use accordingly.
• Pleural infections associated with community acquired pneumonia have different organisms than those with hospital acquired pleural infections.
Community acquired culture negative pleural infection – expected organisms:
• Streptococcus (50%)
• Staphylococcus Aureus
• Haemophilus Influenzae
• Anaerobes (20%)
Initial treatment takes into account these organisms:
• Cefuroxime 1.5 gm tds IV + Metronidazole 500mg tds IV OR
• Meropenem 1g tds IV + Metronidazole 500mg tds IV
Hospital acquired culture negative pleural infection – wider spectrum of organisms
• Staphylococcus Aureus (25%)
• Enterobacteriacae (18%)
• Pseudomonas Aeuroginosa (5%)
• Enterococci (12%)
Initial treatment takes into account these organisms:
o Tazocin 4.5 g qds IV OR
o Ceftazidime 2 g tds IV OR
o Meropenem 1 g tds IV + Metronidazole 500 mg tds IV
+ Teicoplanin 400mg BD for 3 doses then OD for MRSA organisms
2. Which patients require Intercostal tube drainage?
Immediate indications:
• Pus / turbid fluid on aspiration
• Pleural fluid pH <7.2
• Organisms cultured on pleural fluid analysis (Gram stain or culture)
Consider in the following groups:
• Symptomatic – may aid weaning
• Older age (increased risk of subsequent empyema formation)
• Co-morbid disease
• Loculated effusions
• Effusion >50% hemithorax
Repeat pleural aspiration if clinical progress poor – maintain high index of suspicion
3. Which size intercostal tube should be inserted?
• Small catheters (10-14F) as good as larger bore tubes
• Initially insert small bore drain (12-18F - Seldinger)
• If thick pus or initial drain failure with further drain requirement – insert large drain (24-32F)
• Small drains need flushing (30ml Normal Saline every 6h)
4. Should intrapleural fibrinolytics (Streptokinase) be given?
• Not routinely
• Recent evidence from a large Randomised Controlled Trial1 suggests no improved mortality, hospitalisation or surgical rates with Streptokinase use
• There may be a subset of patients who benefit from its use – D/W senior staff
5. Further management
• Ensure adequate nutrition – if oral intake poor or prohibited, enteral or TPN feeding.
• Daily assessment of pleural fluid drainage / markers of sepsis
• If draining <150ml in 24h, repeat CXR
o If persistent pleural collection – consider re-positioning (pulling back) or replacing the tube. Also consider the need for CT scanning.
o If pleural collection resolved and sepsis improved– remove tube and observe.
6. When to refer to thoracic surgeons?
• No definite criteria
• If sepsis fails to respond to tube drainage and antibiotics after 7 days – consider referring to surgeons at that time
• If purulent fluid and loculated collections – more likely to require surgery
• Type of surgery depends on many factors including patients age, co-morbidity and surgeon’s preference
Poor prognostic features with pleural infection (R A P I D)
• Renal profile (Urea >7mmol/l)
• Age >65y
• Protein (albumin<25g/l)
• Inpatient acquired
• Diastolic BP <70mmHg
References
1. Maskell NA, Davies CW, Nunn AJ et al. U.K. Controlled trial of intrapleural streptokinase for pleural infection. N Engl J Med. 2005 Mar 3;352(9):865-74.
2. Paramasivam E, Bodenham A. Pleural fluid collections in critically ill patients BJA 2007; 7: 10-14.
3. BTS Guidelines of the Management of Pleural infections in Adults. Thorax 2003; 58: 18 - 28. www.brit-thoracic.org.uk/bts_guidelines_managepleurdie_html
Dr. S. K. VIJAYAN
INTENSIVE CARE UNIT
WESTON GENERAL HOSPITAL
First Published November 2007
Copyright Priory Lodge Education Limited 2007
Click
on these links to visit our Journals:
Psychiatry
On-Line
Dentistry On-Line | Vet
On-Line | Chest Medicine
On-Line
GP
On-Line | Pharmacy
On-Line | Anaesthesia
On-Line | Medicine
On-Line
Family Medical
Practice On-Line
Home • Journals • Search • Rules for Authors • Submit a Paper • Sponsor us
All pages in this site copyright ©Priory Lodge Education Ltd 1994-


