Surgical Management of Abdominal Wall Hernias in adults - epidemiological aspects and our experiences
Predrag Milosevic1, Marija Kolinovic1
1General Hospital “Danilo I”, Cetinje, Montenegro
Abstract
The goal of our study is to perform a detail epidemiological analysis of the surgical management of abdominal wall hernias in General Hospital “Danilo I”, Cetinje and present our experiences in this field as well as to compare our results with the actual data from the literature.
This retrospective study included 964 patients who underwent surgical treatment for abdominal wall hernia during a 5-year period (from 2005. to 2010.) in a General Hospital “Danilo I” in Cetinje, Montengro.
Data (gender, age, localization and type of hernia and some other characteristics, operative technique, type of anesthesia) were obtained from medical documentation and statistically analyzed.
The study included 741 (76,87%) male and 223 (23,13%) female patients (M:F=3:1).
Total number of surgicaly treated hernias was 1101.
There were 861 (78,20%) primary, 92 (8,36%) recurrent and 148 (13,44%) postoperative hernias.
Two hundred ninety nine (27,16%) hernias were incarcerated (omentum was predominantly incarcerated).
There was statistically significant difference between frequencies of direct and indirect inguinal hernias in patients of both genders (p<0,05). Indirect hernias were more frequent. The difference between frequencies of umbilical and infraumbilical hernias was statistically significant in both genders (p<0,05). Umbilical hernias were more common in men while infraumbilical hernias were more frequent in female patients. Statistically significant difference was found between frequencies of primary and postoperative ventral hernias in patients of both genders (p<0,05). Primary hernias were more common in male patients while postoperative hernias were more frequent in women.
Lichtenstein technique was most commonly performed in hernia repair. Bilateral inguinal hernias were most frequent. Multiple hernias were found in 0,31% of patients. Fourteen (1,45%) of all examined patients were diagnosed with ileus. Appendectomies and cholecystectomies were performed in 0,31% of patients each. Polypropylene mesh extirpation was performed in 2,28% of patients (50% in toto), predominantly in patients with inguinal hernias.
BACKGROUND
Hernia repair is one of the commonest procedures performed by general surgeons. There is no single gold-standard operative technique in hernia repair. (Rutkow IM, 2003) The development of new biological materials has led to a change in the approach to the treatment of hernias. (Liem MSL et al, 1997) Hernia repair now frequently includes implantation of a prosthetic mesh, and this may be done either during open surgery or, increasingly, laparoscopic repair.
One thousand six hundred abdominal wall hernias are operated on in Montenegro annually.
AIM:
The goal of our study was to perform a detail epidemiological analysis of the surgical management of abdominal wall hernias in General Hospital “Danilo I” and present our experiences in this field as well as to compare gained results with the actual data from the literature.
PATIENTS AND METHOD
This retrospective study included 964 patients (older than 17) who underwent surgical treatment for abdominal wall hernia during a 5-year period (from 2005. to 2010.) in a General Hospital “Danilo I” in Cetinje, Montenegro.
Data (gender, age, localization and type of hernia and some other characteristics, operative technique, type of anesthesia) were obtained from medical documentation and statistically analyzed using the GraphPad Prism statistical analysis software.
RESULTS
The study included 741 (76,87%) male and 223 (23,13%) female patients (pts). Male to female ratio was 3 to 1.
Age distribution of patients in the examined group was the following: 286 (29,67%) patients were 65 years old or more, 229 (23,76%) were 55-64 years old, 213 (22,09%) were aged 45-54 years, 108 (11,2%) patients were in the 35-44 year old group, 83 (8,61%) were 25-34 years old and 45 (4,67%) patients were aged 18-24 years.
The percentage of patients who underwent hernia surgery increased with age.
Total number of surgically treated hernias was 1101 (including bilateral herniations).
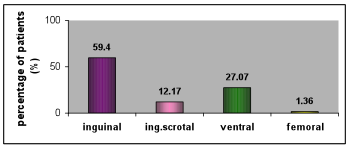
Chart 1. Distribution of hernia localizations
Total number of given anesthesias was 988. Among them 322 (32,59%) were local, 344 (34,82%) spinal, 21 (2,12%) epidural and 302 (30,57%) patients were operated under general anesthesia.
There were 861 (78,20%) primary, 92 (8,36%) recurrent and 148 (13,44%) postoperative hernias (occurred after surgeries excluding herniectomies; among them 6 were recurrent - previously performed herniectomies).
Two hundred ninety nine (27,16%) hernias were incarcerated (predominantly omentum).
The following surgical techniques were performed: Lichtenstein (594 or 53,95% of surgeries), Rives/Stoppa (251 or 22,80% of surgeries), Trabuco (98 or 8,90% of surgeries), Mayo (55 or 4,99% of surgeries), Prolene Hernia System (Johnson & Johnson Co.) (PHS) (37 or 3,36% of surgeries), Bassini/Halstedt (36 or 3,27% of surgeries), Mc-Vay (22 or 2,00% of surgeries), Ferrari (4 or 0,36% of surgeries) and Lotheissen (4 or 0,36% of surgeries). The Lichtenstein technique was most frequently used in hernia repair.
Inguinal hernias
There were 654 (59,40%) inguinal hernias in the examined group of patients (587 in male and 67 in female pts).
There was statistically significant difference in frequency of ingvinal hernias between male and female patients (p<0,05). They were more common in men.
Left-sided inguinal hernias were diagnosed in 292 (44,65%) patients (256 male and 36 female pts) while 362 (55,35%) patients (331 male and 31 female pts) had right-sided hernias.
There was no statistically significant difference between frequencies of right-sided and left-sided inguinal hernias in patients of both genders (p≥0,05).
Recurrent inguinal hernias were found in 60 (9,17%) patients (57 male and 3 female pts) while 594 (90,83%) patients (530 male and 64 female pts) had primary inguinal hernias.
Indirect inguinal hernias were found in 74,63% of female pts and 61,67% of male pts. Direct inguinal hernias were diagnosed in 25,37% of female pts and 31,69% of male pts. Six point sixty four (6,64%) male pts had both, indirect and direct hernias.
The difference between frequencies of direct and indirect inguinal hernias was statistically significant in patients of both genders (p<0,05). Indirect hernias were more common.
Among all inguinal hernias 55 (8,41%) were permagna (48 male and 7 female pts).
Thirty eight (5,81%) hernias were incarcerated (29 male and 9 female pts).
Omentum was most frequently incarcerated, in 23 (60,53%) hernias. Other incarcerated parts of abdominal organs included small intestine (6 or 15,79% of hernias), large intestine (6 or 15,79% of hernias), urine bladder (1 or 2,63% of hernias) and appendix (2 or 5,26% of hernias).

Figure 1. Intraoperative view of incarcerated urine bladder
in patient with right-sided inguinal hernia
Three hundred thirteen (47,86%) surgeries were performed under spinal, 277 (42,35%) under local, 62 (9,48%) under general and 2 (0,31%) surgeries were done under epidural anesthesia. Local and spinal anesthesias were most frequently used for inguinal hernia repairs.
Performed surgical techniques included: Lichtenstein (466 or 71,25% of surgeries), Trabuco (95 or 14,53% of surgeries), application of PHS (34 or 5,2% of surgeries), Bassini/Halstedt (31 or 4,74% of surgeries), Mc-Vay (17 or 2,6% of surgeries), Rives/Stoppa (7 or 1,07% of surgeries) and Ferrari (4 or 0,61% of surgeries). The Lichtenstein technique was most commonly used in inguinal hernia repair.
Inguinoscrotal hernias
One hundred thirty four (12,17%) inguinoscrotal hernias were diagnosed in the examined group of patients. Sixty one (45,52%) were left-sided while 73 (54,48%) were right-sided.
There were 122 (91,04%) primary and 12 (8,96%) recurrent inguinoscrotal hernias.
One hundred twenty nine hernias (96,27%) were indirect and 5 (3,73%) were direct.
Among all inguinoscrotal hernias 96 (71,64%) were permagna.
There were 56 (41,79%) incarcerated inguinoscrotal hernias.
Omentum was most frequently incarcerated, in 33 (58,93%) hernias. Other incarcerated parts of abdominal organs included large intestine (15 or 26,78% of hernias) and small intestine (8 or 14,29% of hernias).


Figure 2. Figure 3.

Figure 4.
Figures 2, 3, 4. The patient is a 67-year-old man with primary right-sided inguinoscrotal and infraumbilical hernias. Surgery was performed under peridural anesthesia, through right inguinoscrotal cut and lower median laparotomy, using the Lichtenstein/Stoppa method (a polypropylene mesh 20x30cm was applied).
Ninty five (70,89%) surgeries were performed under spinal, 20 (14,93%) under local, 18 (13,43%) under general and 1 (0,75%) surgery was done under epidural anesthesia. Spinal anesthesia was most commonly used for inguinoscrotal hernia repair.
Performed surgical techniques included: Lichtenstein (118 or 88,06% of surgeries), Mc-Vay (5 or 3,73% of surgeries), Bassini/Halstedt (5 or 3,73% of surgeries), Trabuco (3 or 2,24% of surgeries), application of PHS (2 or 1,49% of surgeries) and Rives/Stoppa (1 or 0,75% of surgeries). The Lichtenstein technique was most frequently used in inguinoscrotal hernia repair.
Ventral hernias
There were 298 (27,07%) ventral hernias (138 in male and 160 in female pts) in the examined group of patients.


Figure 5. Figure 6.
 Figure 7.
Figure 7.
Figures 5, 6, 7. Male patient with large postoperative anterior abdominal wall hernia (median line), before and after surgery


Figure 8. Figure 9.

Figure 10.
Figures 8, 9, 10. Male patient with large postoperative ventral hernia, before and after surgery
Table 1. Gender distribution of ventral hernia localizations
VENTRAL HERNIA LOCALIZATION |
NUMBER OF PATIENTS |
% |
||
M |
F |
M |
F |
|
umbilical |
69 |
54 |
50 |
33,75 |
supraumbilical |
44 |
30 |
31,88 |
18,75 |
infraumbilical |
12 |
45 |
8,7 |
28,12 |
subcostal |
4 |
11 |
2,9 |
6,88 |
pararectal |
4 |
11 |
2,9 |
6,88 |
lumbal |
4 |
6 |
2,9 |
3,75 |
ileocecal |
1 |
2 |
0,72 |
1,25 |
reg.anus praeter def. |
0 |
1 |
0 |
0,62 |
total |
138 |
160 |
100 |
100 |
There was no statistically significant difference between frequencies of umbilical and supraumbilical hernias in patients of both genders (p≥0,05).
The difference between frequencies of umbilical and infraumbilical hernias was statistically significant in both genders (p<0,05). Umbilical hernias were more common in male while infraumbilical hernias were more frequent in female patients.
Statistically significant difference between frequencies of infraumbilical and supraumbilical hernias was found in patients of both genders (p<0,05). Infraumbilical hernias were more common in female while supraumbilical were more frequent in male patients.
There was no statistically significant difference between frequencies of pararectal and subcostal hernias in both genders (p≥0,05).
There were 148 (49,66%) postoperative (occurred after surgeries excluding herniectomies), 130 (43,62%) primary and 20 (6,71%) recurrent ventral hernias. Among postoperative hernias 6 (4,05%) were recurrent (previously performed herniectomies).
Statistically significant difference between frequencies of primary and postoperative ventral hernias was found in patients of both genders (p<0,05). Primary hernias were more common in male while postoperative hernias were more frequent in female patients.
There were 95 (31,88%) permagna ventral hernias (39 male and 56 female pts).
One hundred ninety four ventral hernias (65,10%) were incarcerated (91 male and 103 female pts).
Omentum was most commonly incarcerated, in 148 (76,29%) hernias. Other incarcerated parts of abdominal organs included: small intestine and omentum (16 or 8,25% of hernias), large intestine and omentum (10 or 5,15% of hernias), small intestine (9 or 4,64%), large intestine (6 or 3,09% of hernias), small intestine, large intestine and omentum (2 or 1,03% of hernias), preperitoneal lipoma (2 or 1,03% of hernias) and fallopian tube, ovary and omentum (1 or 0,52% of hernias).
Twenty one (7,05%) surgeries were performed under local, 17 (5,7%) under spinal, 21 (7,05%) under epidural and 239 (80,2%) surgeries were done under general anesthesia.
General aneshesia was most frequently used for ventral hernia repair.
The performed surgical techniques included: Rives/Stoppa (240 or 80,54% of surgeries), Mayo (55 or 18,46% of surgeries), Lichtenstein (2 or 0,67% of surgeries) and application of PHS (1 or 0,33% of surgeries). The Rives/Stoppa technique was most frequently used in ventral hernia repair.
Femoral hernias
There were 15 (1,36%) femoral hernias in the examined group of patients (7 male and 8 female pts).
Four (26,67%) were left-sided while 11 (73,33%) were right-sided.
Femoral hernias diagnosed in female patients were exclusively right-sided.
All femoral hernias were primary.
Eleven hernias (73,33%) were incarcerated (4 male and 7 female pts). Omentum was incarcerated in 7 (63,64%) and small intestine in 4 (36,36%) patients.
Local anesthesia was used in 7 (46,67%), spinal in 4 (26,67%) and 4 (26,67%) patients were operated under general anesthesia.
The Lichtenstein technique was performed in 8 (53,33%), Rives/Stoppa in 3 (20,00%) and Lotheissen in 4 (26,67%) patients who underwent femoral hernia repair.
Bilateral and multiple hernias
One hundred twenty seven patients (13,17%) were diagnosed with bilateral hernias.
Distribution of bilateral hernia localizations was the following: 2 inguinal (80 or 62,99% of pts), 2 inguinoscrotal (7 or 5,51% of pts), inguinal and inguinoscrotal (13 or 10,24% of pts), inguinal and femoral (4 or 3,15% of pts), inguinal and ventral (11 or 8,66% of pts) and 2 ventral (12 or 9,45% of pts).
Bilateral inguinal hernias were most common. All patients were men. One hundred twenty four (77,5%) hernias were primary while 36 (22,5%) were recurrent.
The following types of bilateral inguinal hernias were found: indirect (26 or 32,5% of pts), direct (27 or 33,75% of pts), indirect and direct (17 or 21,25% of pts), indirect-direct (4 or 5,00% of pts), indirect and indirect-direct (1 or 1,25% of pts) and direct and idirect-direct (5 or 6,25% of pts). Most patients had bilateral direct or bilateral indirect inguinal hernias.
Multiple hernias were found in 3 (0,31%) patients. One patient had bilateral inguinal and right-sided femoral hernia, 1 had bilateral inguinal and supraumbilical hernia and 1 patient was diagnosed with supraumbilical, infraumbilical and right-sided pararectal hernia.
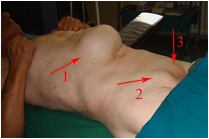
Figure 11. Male patient with bilateral inguinal and
postoperative supraumbilical hernia
Fourteen (1,45%) (8 male and 6 female pts) of all examined patients were diagnosed with ileus. Twelve (85,71%) hernias were primary. One patient had recurrent hernia and one was diagnosed with postoperative hernia. Nine were right-sided while 2 were left-sided.
Localizations of hernias associated with ileus were the following: inguinal (3 or 21,43% of patients), inguinoscrotal (4 or 28,57% of patients), femoral (4 or 28,57% of patients), umbilical (2 or 14,29% of patients) and infraumbilical (1 or 7,14% of patients).
Comorbidities associated with hernias included appendicitis, exacerbation of chronic calculous cholecystitis, scrotal abscess, testicular necrosis, intestinal tumors, abdominal wall phlegmon, varicoceles, uterine prolapse, sygma stenosis, acute orchiepididymitis, phimosis, Douglas abscess, saphena and femoral vein varices, cecal hemangioma, epiploic appendices gangrene. One patient had echinococcal cyst inside hernial sac. Most common were hydroceles which were found in 21 (2,18%) patients. Fourteen were right-sided, 6 were left-sided and 1 patient had bilateral inguinal hernia associated with bilateral hydroceles. Among hernias associated with hydroceles 20 were primary. Thirteen were inguinal and 8 were inguinoscrotal.
Appendectomies were performed in 3 (0,31%) patients (1 female and 2 male pts). One female patient had postoperative infraumbilical hernia associated with chronic appendicitis, 1 male patient had primary umbilical hernia associated with phlegmonous appendicitis and 1 patient was diagnosed with right-sided inguinoscrotal hernia associated with perforative appendicitis.
Cholecystectomies were performed in 3 (0,31%) patients (1 male and 2 female pts). All patients had ventral hernias. One female patient had primary supraumbilical hernia, another had postoperative incarcerated umbilical hernia (omentum and small intestine) and one male patient was diagnosed with postoperative supraumbilical hernia. All 3 patients had exacerbation of chronic calculous cholecystitis.
Hernia surgery complications
Early postoperative complications included wound dehiscence, seroma, genitofemoral nerve incarceration, hematoma, polypropylene mesh infection.
Polypropylene mesh extirpation was performed in 22 (2,28%) patients (18 male and 4 female pts).
Age distribution of patients who underwent polypropylene mesh extirpation was the following: 59,09% of patients were more than 60 years old, 22,73% were aged 50-60 years, 13,64% were in the 40-50 year old group and 4,54% of patients were 30-40 years old.
Eleven (50%) polypropylene meshes were extirpated in toto.
Fourteen (63,64%) inguinal, 5 (22,73%) umbilical, 2 (9,09%) pararectal and 1 (4,54%) supraumbilical hernias were associated with postoperative mesh extirpation.
Inguinal hernias were most frequent in patients who underwent postoperative extirpation of polypropylene mesh. All patients were men.
DISCUSSION:
Approximately 75% of all hernias occur in the inguinal region. (Katz DA, 2001) In 1979, three-fourths of the abdominal wall hernias operated on in the US were inguinal. From a total of 686 000 operated hernias, 500000 were inguinal (73%), 65000 umbilical (9,5%), 43000 incisional (6,2%), 19000 femoral (2,7%) and 59000 were other types of hernias (8,6%). (Bendavid R et al, 2001)
In our study, 59,40% of all hernias were inguinal, 11,17% umbilical, 13,44% incisional, 1,36% femoral and 14,63% were other types of hernias.
The percentage of patients who undergo hernia surgery increases with age. Out of the total repairs performed in the US in 1996, 18% were on patients under 15 years of age, 29% in the 15-44 age group, 23% in the 45-64 age group and 30% in the over 65 age group. (Bendavid R et al, 2001)
Our study included adult patients (older than 17) and we report the folowing percentages: 24,48% of pts in 18-44 age group, 45,85% in 45-64 age group and 29,67% in the group of patients older than 65.
It is a well-known fact that the male population is more frequently affected with inguinal hernias than the female, but the true proportion is unknown. Various authors report different figures. Malgaigne in 1841, in the first statistical study about the distribution of inguinal hernia in the general population according to sex reports male to female ratio 4:1, El-Qaderi 8,2:1, Wantz 25:1. The large differences among series of patients probably reflect the difference in the number of patients, as well as the various racial, genetic, nutritional and other differences in the populations studied. (Bendavid R et al, 2001)
In our study, there were almost 9 times more male than female patients with inguinal hernias.
The percentage of men who underwent inguinal hernia repair was 89,75%, which corresponds to data in the literature (almost 90%). (Matthews RD et al, 2008)
In the examined group of patients with inguinal hernias, approximately two thirds of hernias were indirect and one third were direct. Indirect hernias were more frequent in patients of both genders. This also corresponds to data from the literature. (Katz DA, 2001)
The total number of recurrent inguinal hernia repair is around 10% (goes from 0,2% to 15%). (Bendavid R et al, 2001) In our study, the percentage of recurrent inguinal hernias was 9,17%.
Bilateral inguinal hernias occur in up to 20% of adult patients. (Goroll AH et al, 2005) In the examined group, 13,94% of patients were diagnosed with these hernias.
Inguinal hernia may display very unusual sac contents. Appendix, ovary, fallopian tube and urinary bladder have been rarely reported. (Gurer A et al, 2006) It is estimated that inguinal hernial sac contains an uninflamed appendix in approximately 1% of patients with inguinal hernia. (D'Alia C et al, 2003, Lyass S et al, 1997) New studies report lower percentages, 0,38% (Ballas K et al, 2009), 0,51% (Gurer A et al, 2006).
In the examined group of patients with inguinal hernias, appendix was found inside hernial sac in 0,3% of patients.
One patient had right-sided inguinal hernia with urinary bladder in the hernial sac. About 1%–4% of all inguinal hernias involve the bladder. The incidence may reach 10% among obese men aged 50 to 70 years. (Fisher PC et al, 2004, Huerta S et al, 2005) Most cases are asymptomatic and are usually found incidentally on radiographic imaging or intraoperatively. Bladder involvement in inguinal hernias is often not recognized before surgical repair. Less than 7% are diagnosed preoperatively, 16% are diagnosed postoperatively because of complications and the remainder of cases are diagnosed perioperatively. (Watson LF, 1948) The risk of bladder injury during surgery has been reported as 12%. (Catalano O, 1997) Therefore, it is so important to establish an accurate diagnosis of these hernias.
Our patient did not report any urinary symptoms (2-stage urination with manually compression of bladder for complete emptying). Therefore the diagnosis was established intraoperatively. Postoperative recovery was uneventful, and all symptoms resolved.
In the examined group of patients with inguinal hernias, local anesthesia was used for high percentage of surgeries (42,35%). It is a preferred choice of anesthesia for all reducible adult inguinal hernia repairs. It is safe, simple, effective, and economical, without post-anesthesia side effects. Furthermore, local anesthesia administered before the incision produces longer postoperative analgesia because local infiltration, theoretically, inhibits build-up of local nociceptive molecules, leading to better pain control in the postoperative period. (Amid PK et al, 1994)
The Lichtenstein technique was most commonly performed in inguinal hernia repair, which corresponds to data from the literature. (De Lange DH et al, 2009)
In May 2008, in our hospital, we started using the Prolene Hernia System (PHS, Johnson & Johnson Co.) in inguinal hernia repair. Till January 2010, 34 PHSs were applied. The study aimed to compare outcomes of Prolene Hernia System repair and the gold standard Lichtenstein on-lay mesh repair of inguinal hernias (Awad SS et al, 2007) revealed decreased overall complication rates with significantly less seroma and hematoma rates in patients who underwent PHS repair. Therefore, the PHS repair may represent a superior alternative for the repair of inguinal hernias. But this needs further investigation.
Umbilical hernias constituted 11,17% of all hernias in the examined group. Male to female ratio among patients with these hernias was 1,3:1. Some authors report ratio 1:1,7 in favour of women. (Ruhl CE et al, 2007)
The percentage of postoperative primary (96,1%) and recurrent (3,9%) ventral hernias closely corresponds to data from the literature (95,1% and 4,9%). (Bisgaard T et al, 2009)
Female to male ratio among patients with postoperative ventral hernias was 2,2:1, which also matches data from the literature. (Ruhl CE et al, 2007)
In the near future we may see a reduction in incisional hernias due to the advent of laparoscopic surgery. But this may lead to a new class of hernias - trocar site hernias. (Bendavid R et al, 2001)
Femoral hernias are relatively rare, making up 2-8% of all adult groin hernias. (Waddington RT, 1971, Maingot R, 1968) In the examined group of patients, 1,36% of all surgically treated hernias were femoral. They were incarcerated in 73,33% of patients which maches data from the literature according to which these hernias are most frequently incarcerated abdominal hernias. (David T, 1967)
Hydroceles may be associated with hernias, especially on the right side of the body. (A Garriga V et al, 2009) In our study, 2,18% of patients were diagnosed with hydrocelas among which 66,67% were right-sided.
During a 5-year period (60 months), 22 polypropylene meshes were extirpated, among which 11 (50%) in toto. The study conducted in Italy reports the surgical extirpation of 32 meshes, during 40 months, among which 22 (68,75%) were extirpated in toto. (Tolino MJ et al, 2009)
CONCLUSIONS
1. Inguinal hernias were most common in the examined group of patients.
2. Primary hernias were most frequent.
3. Twenty seven point sixteen percent (27,16%) of hernias were incarcerated
(predominantly omentum).
4. The Lichtenstein technique was most frequently used in hernia repair.
5. There was statistically significant difference in frequency of ingvinal hernias between
male and female patients (p<0,05). They were more common in men.
6. There was no statistically significant difference between frequencies of right-sided and
left-sided inguinal hernias in patients of both genders (p≥0,05).
7. The difference between frequencies of direct and indirect inguinal hernias was
statistically significant in patients of both genders (p<0,05). Indirect hernias were more
common.
8. The Lichtenstein technique was most commonly used in inguinal hernia repair.
9. Inguinoscrotal hernias constituted 12,17% of all hernias in the examined group.
10.Seventy one point sixty four percent (71,64%) of inguinoscrotal hernias were
permagna and 41,79% were incarcerated.
11.The Lichtenstein technique was most frequently used in inguinoscrotal hernia repair.
12.Ventral hernias constituted 27,07% of all hernias in the examined group.
13.There was no statistically significant difference between frequencies of umbilical and
supraumbilical hernias in patients of both genders (p≥0,05).
14.The difference between frequencies of umbilical and infraumbilical hernias was
statistically significant in both genders (p<0,05). Umbilical hernias were more
common in male while infraumbilical hernias were more frequent in female patients.
15.Statistically significant difference between frequencies of infraumbilical and
supraumbilical hernias was found in patients of both genders (p<0,05). Infraumbilical
hernias were more common in female while supraumbilical were more frequent in
male patients.
16.There was no statistically significant difference between frequencies of pararectal and
subcostal hernias in both genders (p≥0,05).
17.Postoperative ventral hernias were most common.
18.Statistically significant difference between frequencies of primary and postoperative
ventral hernias was found in patients of both genders (p<0,05). Primary hernias were
more common in male while postoperative hernias were more frequent in female
patients.
19.The Rives/Stoppa technique was most frequently used in ventral hernia repair.
20.Femoral hernias constituted 1,36% of all hernias in the examined group.
21.Femoral hernias diagnosed in female patients were exclusively right-sided.
22.All femoral hernias were primary.
23.Seventy three point thirty three percent (73,33%) of femoral hernias were
incarcerated.
24.The Lichtenstein technique was performed in 53,33% of femoral hernia surgeries.
25.Bilateral hernias were found in 13,17% of patients in the examined group.
26.Bilateral inguinal hernias were most common. All patients were men.
27.Multiple hernias were found in 0,31% of patients in the examined group.
28.One point forty five percent (1,45%) of all examined patients were diagnosed with
ileus.
29.Hydroceles were found in 2,18% of patients in the examined group.
30.Appendectomy and cholecystectomy were performed in 0,31% of patients,
respectively.
31.Polypropylene mesh was extirpated in 2,28% of patients (50% in toto), mostly in
male patients with inguinal hernias.
REFERENCES
1. Rutkow IM. Demographic and socioeconomic aspects of hernia repair in the United States in 2003. Surg Clin North Am. 2003; 83:1045–1051.
2. Liem MSL, Van Der Graaf Y, Van Steensel CJ, et al. Comparison of conventional anterior surgery and laparoscopic surgery for inguinal hernia repair. N Engl J Med 1997; 336:1541–7.
3. Katz DA. Evaluation and management of inguinal and umbilical hernias. Pediatr Ann. 2001; 30(12):729-35.
4. Bendavid R et al. Abdominal wall hernias: principles and management. 1st ed. New York: Springer; 2001, 110-112.
5. Matthews RD, Neumayer L. Inguinal hernia in the 21st century: an evidence-based review. Curr Probl Surg. 2008; 45(4):261-312.
6. Goroll AH, Mulley AG. Primary care medicine: office evaluation and management of the adult patient. 5th ed. Philadelphia, Lippincott Williams & Wilkins; 2005:431-434.
7. Gurer A, Ozdogan M, Ozlem N, Yildirim A, Kulacoglu H, Aydin R. Uncommon content in groin hernia sac. Hernia. 2006; 10:152-155.
8. D'Alia C, Lo Schiavo MG, Tonante A, Taranto F, Gagliano E, Bonanno L, Di Giuseppe G, Pagano D, Sturniolo G: Amyand's hernia: case report and review of the literature. Hernia 2003;7:89-91.
9. Lyass S, Kim A, Bauer J: Perforated appendicitis within an inguinal hernia: case report and review of the literature. Am J Gastroenterol 1997;92:700-702.
10. Ballas K, Kontoulis Th, Skouras Ch, Triantafyllou A, Symeonidis N, Pavlidis Th, Marakis G, Sakadamis A. Unusual findings in inguinal hernia surgery: Report of 6 rare cases. Hippokratia 2009; 13(3):169-171.
11. Fisher PC, Hollenbeck BK, Montgomery JS, et al. Inguinal bladder hernia masking bowel ischemia. Urology 2004; 63:175-6.
12. Huerta S, Fairbanks T, Cinat M. Incarcerated vesicoinguinal hernia presenting with gross hematuria. J Am Coll Surg 2005; 201:992-3.
13. Watson LF. Hernia. 3rd ed. St. Louis (MO): CV Mosby, 1948: 476-486.
14. Catalano O. Ultrasound evaluation of inguinoscrotal bladder hernias: report of three
cases. Clin Imaging 1997; 21:126-8.
15. Amid PK, Shulman AG, Lichtenstein IL. Local anesthesia for inguinal hernia repair step-by-step procedure. Ann Surg. 1994; 220(6):735–737.
16. De Lange DH, Kreeft M, Van Ramshorst GH, Aufenacker TJ, Rauwerda JA, Simons MP. Inguinal hernia surgery in the Netherlands: are patients treated according to the guidelines? 2009. Hernia. 2. Nov. 2009
<http://www.springerlink.com/content/ttjh4012h54v772w>
17. Awad SS, Yallampalli S, Srour AM, Bellows CF, Albo D, Berger DH, Michael E, DeBakey VAMC. Improved outcomes with the Prolene Hernia System mesh compared with the time-honored Lichtenstein onlay mesh repair for inguinal hernia repair. Am J Surg 2007; 193(6):697-701.
18. Ruhl CE, Everhart JE. Risk factors for inguinal hernia among adults in the US population. Am J Epidemiol. 2007; 165(10):1154-61.
19. Bisgaard T, Kehlet H, Bay-Nielsen MB, Iversen MG , Wara P, Rosenberg J, Friis-Andersen HF, Jorgensen LN. Nationwide study of early outcomes after incisional hernia repair. British Journal of Surgery 2009; 96(12):1452-1457.
20. Waddington RT. Femoral hernia: a recent appraisal. Br J Surg 1971; 58:920-922.
21. Maingot R. The choice of operation for femoral hernia, with special reference to McVay's technique. Br J Clin Pract 1968; 22:323-329.
22. David T. Strangulated femoral hernia. Med J Aust 1967; 1:258.
23. A Garriga V, Serrano A, Marin A, Medrano S, Roson N, Pruna X. US of the Tunica Vaginalis Testis: Anatomic Relationships and Pathologic Conditions. Radiographics. 2009; 29(7):2017-2032.
24. Tolino MJ, Tripoloni DE, Ratto R, Garcia MI. Infections associated with prosthetic repairs of abdominal wall hernias: pathology, management and results. Hernia 2009; 13(6):631-637.
Copyright Priory Lodge Education Limited 2010
First Published September 2010
All pages copyright ©Priory Lodge Education Ltd 1994-


