Lemierre’s Syndrome: An Unusual Manifestation |
|---|
Derek Park MRCS (Eng)1 Kia Rezajoi FRCS2
1Royal National
Orthopaedic Hospital, Stanmore HA7 4LP, UK
2Great Ormond Street Hospital for Children, London WC1N 3JH, UK
Lemierre’s syndrome is caused by an acute oropharyngeal infection with secondary septic thrombophlebitis of the internal jugular vein and frequent metastatic infections. There has been a resurgence in this rare condition in recent years, some attributed to the decreased use of antibiotics to treat oropharyngeal infection, but many clinicians remain unaware of the condition (1). We present a case of Lemierre’s syndrome complicated by an epidural abscess. Oropharyngeal infection is perhaps one of the commonest presentations to a General Practitioner and through this case report we hope to increase awareness of this condition and presenting a previously unreported complication of Lemierre’s syndrome.
CASE HISTORY
A 43 year old woman presented with a 2 day history of neck and back pain and a 1 day history of acute confusion with weakness in both legs. She initially presented to her general practitioner with a 3 week history of a sore throat, fever and swollen neck glands and was treated with a course of eryhthromycin. The patient had otherwise been healthy with no past medical history of note and no recent overseas travel history.
On admission she was confused, agitated, febrile and tachycardic. Examination of the chest revealed decreased air entry in her lower lobes bilaterally. A neurological examination of the patient revealed flaccid lower limbs with reduced power MRC grade 1 and diminished reflexes bilaterally. Her upper limbs were normal and cranial nerve examination was unremarkable. The patient had a neutrophilia and a markedly elevated CRP of 396.5.
MRI scanning demonstrated a collection lying anterior to the spinal cord extending from C1 caudally to T5, a posteriorly placed epidural collection extending from T3-4 to approximately T5, and a further collection extending from T11 to L3. (figure 1&2) CT scan of the chest, abdomen and pelvis revealed bilateral lower lobe consolidation and effusions (figure 3), and low density areas within both psoas muscles consistent with small abscesses.

Figure 1 Epidural abscess extending from C1 caudally to T5

Figure 2 Epidural collection extending from T11 to L3
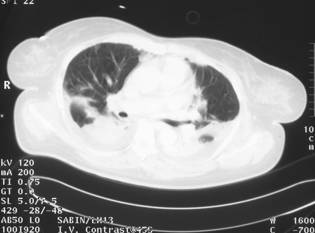
Figure 3 CT scan of the chest showing bilateral lower lobe consolidation and effusions
A T9 laminectomy was performed which revealed an epidural abscess from which 3-4 mls of pus was drained. 24 hours later an anterior C3 foraminotomy was performed and evacuation of pus from an epidural and intradural abscess was performed. Polymerase chain reaction of the pus grew fusobacterium necrophorum and the patient was started on fluconazole, metronidazole, and meropenem. Postoperatively the patient regained power in her upper limbs, however there was no significant change in her lower limbs at 3 weeks post operatively.
COMMENT
Lemierre’s syndrome is caused by the anaerobic bacterium, Fusobacterium necrophorum and typically affects healthy teenagers and young adults. The infection originates in the oropharynx and spreads haematogenously via a septic thrombophlebitis of the internal jugular vein. Sites of septic embolism have been described in the lung, joints, and bones.
Lemierre’s syndrome was described by Andre Lemierre in 1936 who published a series of 20 patients in the Lancet (2). Lemierre described a group of "anaerobic postanginal septicaemias" that was characterized by anaerobic septicaemia, internal jugular vein thrombosis, and septic emboli that arose secondary to infections of the head and neck, particularly in the oropharynx. The disease entity was relatively common in the preantibiotic era, however with the widespread use of antibiotics the prevalence declined and the syndrome is often overlooked when it appears today (3). There has been a resurgence of publications in the cited literature since 1990, with recent data suggesting that the incidence is rising (4). The typical clinical picture is characteristic but the diagnosis is often overlooked due to lack of awareness of the condition. To our knowledge this is the first reported case of Lemierre’s syndrome involving the epidural space.
REFERENCES
- T Riordan, M Wilson. Lemierre’s syndrome: more than a historical curiosa. Postgraduate Medical Journal2004;80:328-334
- Lemierre A. Septicaemias and anaerobic organisms. Lancet 1936;i:701–3.
- Moore-Gillon J, Lee TH, Eykyn SJ, Phillips I. Necrobacillosis: a forgotten disease. BMJ1984; 288:1526-1527
- Brazier JS, Hall V, Yusuf E, et al. Fusobacterium necrophorum infections in England and Wales 1990–2000. J Med Microbiol 2002;51:269–72
All pages copyright ©Priory Lodge Education Ltd 1994-2006.