A. De,1 K. Birch,2 J. Nolan,3
C.J. Peden3
1. Senior House Officer
2. Advanced Trainee in Intensive Care Medicine
3. Consultant in Anaesthesia and Intensive Care MedicineDepartment of Anaesthesia
and Intensive care Medicine
Royal United
Hospital
Combe Park
Bath
BA1 3NG
Correspondence to: A. De
E mail fordyce11b@yahoo.com
Summary
We describe a case of a 19 year old man who developed traumatic pulmonary pseudocysts
after a roll-over road traffic crash. These were associated with significant
pulmonary haemorrhage requiring a period of mechanical ventilation, but resolved
without specific intervention. Review of the literature confirms that this rare
complication of blunt chest trauma occurs usually in young adults and, although
normally benign, can be associated with life-threatening haemoptysis and secondary
infection.
Keywords
Trauma, Blunt, Pulmonary, Cyst, Lung injury
Introduction
The strict pathophysiological definition of traumatic pulmonary contusion is
exudation of fluid and blood into the lung parenchyma without substantial tissue
disruption. Rarely, chest trauma can cause pulmonary pseudocysts: air, fluid,
or blood filled, well defined spaces not lined with epithelium. This complication
of blunt chest trauma has been described previously in a few case reports and
case series, but mainly in surgical1-7 and radiological8-12 journals. We describe
the occurrence of traumatic pulmonary pseudocysts in a young man.
Case Report
A 19 year old man was admitted to hospital after a road traffic crash: he was
the driver of a car, which overturned at 60 mph. He lost consciousness for approximately
1 minute. On arrival in the emergency department his airway was clear. His oxygen
saturation by pulse oximetry (SpO2) was 100% while breathing 15 litres of oxygen;
he had a respiratory rate of 24 per minute, the trachea was central, and on
auscultation he had breaths sounds equally on both sides but with some scattered
coarse crackles; he had some haemoptysis but did not complain of chest pain.
His heart rate was 100 and blood pressure was 130/90. His GCS was 14. He was
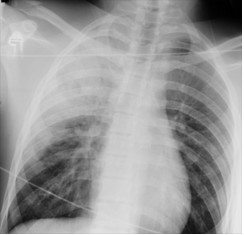
agitated. Initial examination of the abdomen was normal. Chest radiograph revealed
infiltrates in the upper zone of the right lung, fluid in the horizontal fissure
and fracture of the right clavicle (Figure 1).
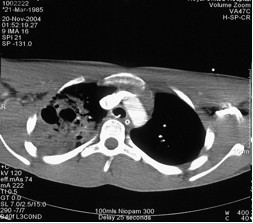
He was very aggressive and agitated so he was sedated and intubated before transfer to the computed tomography (CT) scan room. CT scans of the brain and spine were normal but the chest CT showed extensive consolidation in right upper lobe with air bronchograms and marked cavitation (Figure 2). There was also patchy consolidation of right and left lower lobe, possibly due to aspiration, and a small pneumothorax on the right. He was admitted to the intensive care unit (ICU) for ventilation with a diagnosis of pulmonary contusion and aspiration. Over the next 48 hours, he had several episodes of frank bleeding through the tracheal tube, mostly when the sedation was reduced for neurological assessment and possible extubation. We were concerned that the cavities in the upper zone of the right lung, combined with significant haemoptysis, might represent active tuberculous (TB). Thorough questioning of the patient’s parents ruled out any obvious risk factors for TB; he was a perfectly healthy young man. Sputum was sent for acid fast bacilli and microbial culture and sensitivity; nothing of significance was identified or grown from these samples.
On day 3, a repeat chest CT was similar to the previous CT; however, the right upper lobe consolidations with air filled cavities were considered to be consistent with traumatic pulmonary pseudocysts and intrapulmonary haemorrhage. The patient was finally extubated on day 4 and maintained adequate oxygenation with 60% high flow oxygen by facemask. His oxygen requirements reduced rapidly over the next two days and he was able to mobilise without being breathless. On day 8 he was discharged from ICU.
Discussion
In comparison with intrapulmonary haematoma or pulmonary contusion, traumatic
pulmonary pseudocysts are rare: a tertiary centre in Milan recently reported
traumatic pulmonary pseudocysts in 10 patients over nine years.1 Two mechanisms
have been suggested for the development of pseudocysts; both involve exposure
of the lungs to significant forces, such as those generated during high speed
road traffic crashes. Firstly, sudden compression of an area of lung closes
off a segment of the peripheral bronchial tree and creates a bursting pressure
within it. The enclosed airspace is then expanded by the rupture of alveolar
walls.10 A second possible mechanism is through the propagation of concussion
waves, which create shearing stresses that tear the substance of the lung.11
Children and young adults seem to be particularly vulnerable, probably because
of the great flexibility of their thoracic walls, which enables the visceral
pleura to remain intact despite massive forces applied to the lung parenchyma;
one study reported that 85% of patients with traumatic pulmonary pseudocyst
were younger than 30 years.9 In a recent series from Greece, all 14 patients
developing traumatic pulmonary pseudocysts were under 25 years.2
Traumatic pulmonary pseudocysts appear as single or multiple, oval or spherical
lesions, varying in size from 2 to 14 cm diameter.13 Approximately half present
as thin walled air spaces, with or without a fluid level.6 In adults, the chest
radiograph appearances may be similar to those of a lung abscess, tuberculosis
or cavitating bronchial carcinoma.9 In children, the lesion may be confused
with a pneumatocele, pulmonary cyst or pulmonary sequestration.7,9
Traumatic pulmonary pseudocysts may be identified on plain radiographs: an air
fluid level may be visible, surrounded by consolidated lung due to pulmonary
contusion; however, a CT scan is much better for detecting these lesions. In
one series of ten patients with traumatic pulmonary pseudocysts identified on
CT scans, none were detectable on plain chest radiograph.1 Radiological resolution
of the pseudocysts occurs usually in 2-3 months.2,4,5
Traumatic pulmonary pseudocysts can be asymptomatic or associated with pain,
haemoptysis and dyspnoea.2,14 They are usually benign lesions that do not require
specific therapy. The haemoptysis is not usually life threatening, but there
has been at least one reported case in which emergency lobectomy was required
to control endobronchial bleeding.1 Our patient had significant haemoptysis
requiring a period of mechanical ventilation and high concentration of oxygen,
but it resolved without surgical intervention. Prophylactic antibiotic therapy
is not necessary; however, secondary infection with abscess formation has been
described and may need surgical or percutaneous drainage.15,16
References
1. Melloni G, Cremona G, Ciriaco P, et al. Diagnosis and treatment
of traumatic pulmonary pseudocysts. J Trauma 2003; 54: 737-43.
2. Athanassiadi K, Gerazounis M, Kalantzi N, Kazakidis P, Fakou A, Kourousis
D. Primary traumatic pulmonary pseudocysts: a rare entity. Eur J Cardiothorac
Surg 2003; 23: 43-5.
3. Stathpoulos G, Chrysikopoulou E, Kalogeromitros A, et al. Bilateral traumatic
pseudocysts: case report and literature review. J Trauma 2002; 53: 993-6.
4. Moore FA, Moore EE, Haenel JB, Waring BJ, Parsons PE. Post-traumatic pulmonary
pseudocyst in the adult: pathophysiology, recognition, and selective management.
J Trauma 1989; 29: 1380-5.
5. Kato R, Horonouchi H, Maenaka Y. Traumatic pulmonary pseudocyst: report of
12 cases. J Thorac Cardiovasc Surg 1989; 97: 309-12.
6. Santos GH, Mahendra T. Traumatic pulmonary pseudocyst. Ann Thoracic Surgery
1979; 27: 359-62
7. Blane CE, White SJ, Wesley JR et al. Immediate traumatic pulmonary pseudocysts
formation in children. Surgery 1981; 90: 872-5.
8. Robin J, White R. Formation and resolution of bilateral traumatic pulmonary
pseudocysts. Australas Radiol 1995; 39: 292-5.
9. Sorsdahi OA, Powell JW. Cavitary pulmonary lesions following non-penetrating
chest trauma in children. Am J Roentgenol 1965; 95:118-24.
10. Fagan CJ. Traumatic Lung Cyst. Am J Roentgenol 1966; 97: 186.
11. Willams JR, BonteFJ. Pulmonary damage in non-penetrating chest injuries.
Radiol Clin North Am 1963; 1: 439.
12. Fagan CJ, Swischuk LE. Traumatic Lung and paramediastinal pneumatoceles.
Diag Radiol 1976; 120: 11-8.
13. Shirakusa T, Araki Y, Tsutsui M, et al. Traumatic Lung Pseudocyst. Thorax
1987; 42: 516-9.
14. Stultz P, Schmitt HE. Hasswe J, Gardel E. Traumatic pulmonary pseudocysts
and paramediastinal air cyst. Two rare complications of blunt chest trauma.
J Trauma 1984; 24: 850-3.
15. Gincherman Y, Luketich JD, Kaiser LR. Successful nonoperative management
of secondarily infected pulmonary pseudocyst: case report. J Trauma 1995; 38:
960-3.
16. Caroll K, Cheeseman SH, Fink MP, Umali CB, Cohen IT. Secondary infection
of post-traumatic pulmonary cavitary lesions in adolesecents and young adults:
role of computed tomography and operative debridement and drainage. J Trauma
1989; 29: 109-12.
Figure 1. Initial chest radiograph showing infiltrates in the right
upper zone; cystic changes are just visible. There is a fracture of the right
clavicle.
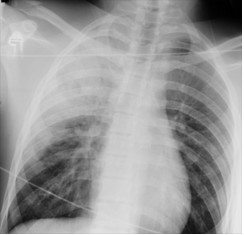
Figure 2. Computed tomography of the chest. Two large cysts are surrounded by
several smaller cysts.
All pages copyright ©Priory Lodge Education Ltd 1994-2006.