THE EFFECT OF LUTING AGENT
ON THE FRACTURE RESISTANCE OF
ALL-CERAMIC CROWNS
![]()
![]()
The mean compressive loads to failure were 464 N, 495 N and 535 N for GP1, GP 2, GP 3 and 1340 N for the control group. All results indicated that superior fracture resistance was obtained when dentine bonding was incorporated into the luting procedure together with etching of the ceramic fitting surface and the use of a resin-based luting material.
It is concluded that when all-ceramic crowns were loaded to failure on prepared dentine surface, higher fracture strength results were obtained when a composite resin luting agent was used.
1. INTRODUCTION
As a result of increasing patient awareness of dental aesthetics and fear of potential allergic, electrochemical and toxic effects of amalgam, more and more patients prefer metal-free tooth-coloured restorations even in their posterior teeth, as the enhanced appearance of crowns that do not have the metal component may be of great importance to improve aesthetic concerns. Restorations must not only provide satisfactory aesthetics, but also satisfactory functional properties. The use of composite restorations in posterior teeth is still controversial and although the initial marginal adaptation of occlusal composite restorations can be improved by bevelling the enamel margins and using an incremental placement technique,1 a decline in marginal integrity must be expected if the main occlusal contacts are located on the restoration.2 For this reason, the use of all-ceramic restorations in the posterior region of mouth is increased.
Ceramics have been used for tooth restoration for a long time. The French chemist Duchateau first suggested the use of ceramics for a dental appliance in 1776.3 Single jacket crowns were the first all-ceramic restorations developed by Land in the last century for the restoration of severely damaged teeth. Although conventional jacket crowns have been improved so that they can offer excellent clinical results, their strength still remains fairly low and it is difficult to obtain a reproducible marginal fit. The material being a glass lacks any fracture toughness. Porcelain jacket crowns are extremely sensitive to the presence of surface micro-cracks and its use is restricted only to low-stress bearing areas. This type of crown was well accepted until the advent of the porcelain-bonded-to-metal crown in the 1960's.3
Porcelain fused to metal crown also presented disadvantages. Oxidation and corrosion products resulting from the fired alloys, led to reduced tissue compatibility. The presence of the metal collar in the
cervical area compromises the aesthetic result of the restoration. In addition, the crown may appear opaque and less vital because of inadequate light transmission due to metal which obscures the transmission of light.4,5. Therefore the desire for better aesthetics and improved biocompatibility led to the development of higher strength all-ceramic restoration systems.However, based on the fact that ceramic materials are, in general, brittle, and that fracture is the only catastrophic mode of failure, it appears necessary to find a ceramic material which may considered to promote strength and high aesthetics. The new technology and materials brought about a renaissance of the all-ceramic crown in the early 1980's.
2. SCIENTIFIC BACKGROUND
2.1 Development of all-ceramic systems
Pioneers in the development of all-ceramic restorations are indisputably the Cerestore (Johnson and Johnson Dental Care Co.) and Dicor (Dentsply International) systems.3 Inspired by their aesthetic possibilities, a variety of ceramics soon followed for the fabrication of crowns, inlays and veneers. These were marked under such names as Hi-Ceram (Vivadent) and Optec (Jeneric/Pentroninc). Dicor followed the technique of heat-treatment (ceramming) in which among other things, mica crystals are formed with the use of conventional lost-wax process. Cerestore was based on the technique of injection moulding to fabricate ceramic copings. The development of these new ceramic materials nourished hopes that the construction of all-ceramic of high strength could be possible. However, not withstanding the advantages of biocompatibility and improved aesthetics, all the expectations were not fulfilled. It is well known that the problems of ceramic materials is their brittleness and lack of resistance against excessive tensile forces.
The atomic structure of the ceramic materials would suggest achievement of high strength but this expectation cannot be fulfilled in practice. Microscopic surface defects under load lead to fracture progression and spontaneous failure. As a consequence, the search for new techniques has continued. In-Ceram (Vita Zahnfabrik) was developed by Sadoun in France 6 and uses alumina in a slip-casting procedure as a core material. The core material replaces the metal framework of porcelain fused to metal crown. The slip-casting alumina is first sintered in a furnace yielding a porous framework that is then infiltrated with molten glass in a second firing process. The combination of these two properties gives the material its outstanding properties. Because of the very densely packed alumina particles, crack propagation from different defect sites is limited. The glass infiltration, eliminates almost all the porosities which constitute points of weakness in ceramics. In that way, both procedures contribute to a flexural strength which is the highest ever reported for dental ceramics.7,8
Recent research has shown that great improvements in the fracture strength of ceramics are possible by the use of glass-infused alumina. It has been shown by several studies that the glass infiltrated aluminium oxide ceramic, In-Ceram, has a 3 to 4 times higher strength than other ceramic or glass materials.9
2.2 Glass-ceramics and the development of IPS-Empress system
The use of glass-ceramics for fabrication of all-ceramic crowns offers the possibility to improve the strength of the respective material by decreasing fracture progression. Stookey successfully developed a new group of materials called glass-ceramics by controlling the crystallisation of the special glasses.10 Glass is an undercooled liquid with an amorphous, non-crystalline structure. In traditional manufacturing of glass-ceramics, a base glass is heat-treated and cooled slowly to produce crystals embedded in a glass-matrix. This procedure has a number of stages which finally permits the production of a special glass formed by controlled crystallisation.10 There are two forms of controlled crystallisation. Some systems are subject to surface nucleation e.g. Dicor, and others to volume (bulk) nucleation e.g. IPS-Empress. The conventional glass-ceramic material (Dicor) until now has been produced by a crystallisation within the glass, known as volume crystallisation. In this, crystals of almost the same size and morphology develop in the base glass by uniform dispersion. Stages of nucleation and crystallisation take place simultaneously and represents the necessary scientific prerequisites for the fabrication of a glass-ceramic.
In contrast, glass-ceramics based on the leucite system such as IPS-Empress cannot be cerammed by controlled volume crystallisation.10 In this case, another approach must be applied. First, a base glass is melted. Subsequently, it is heat-treated to initiate nucleation and primary crystallisation and then ground. In the first stage, the raw glass granules are heated to 960*C and held for a specific heating at this temperature. As a result, controlled nucleation appears from the grain boundary toward the centre of the grain. In the second stage, a further heat-treatment takes place at 1180 Centigrade which produces a fine dispersion of crystals.1,10
The semi-finished product in powder form is pressed into cylinders and fired, resulting in the ceramic ingots. The base glass differs significantly from the glass used in traditional volume crystallisation.
Nucleation and crystallisation coincides for a lesser period of time than in volume crystallisation. For this reason, a new mechanism of controlled crystallisation is used. Crystals grow directly inward from the surface of the glass-matrix. This primary process of nucleation and crystallisation in the base glass is characterised by the initiation of nucleation phase at the grain boundary of the ground glass. Heating of the base glass produces small leucite crystals which, at the beginning, are highly disordered crystallochemically. The growth of leucite crystals proceeds from the centre of nucleation outwards.3,10 In this way, crystals may form flower-like design petals. The leucite crystals continue their growth during the subsequent stage of glass-ceramic ingot processing. As a result, further maturing of the leucite crystals takes place during dental laboratory procedures. After crystal formation and maturing, leucite crystals demonstrate uniform growth. The improved strength of the leucite reinforced glass-ceramic material results from the better dispersion of crystals in the glass-matrix. Because of the difference in density and coefficient of thermal expansion, between the glass-matrix and the crystals, stress formation is produced which separates crystals from the glass particle. This separation is particularly important for the reinforcement of the glass material by dispersion.1,10 The thermal expansion coefficient of glass is far lower than that of crystals. Therefore, as the material solidifies (cooling stage) the presence of a high expansion coefficient crystal in a matrix of a lower expansion coefficient glass, generates tangential compressive stresses in the glass and radial stresses within the leucite crystals.3
During the final phase of contraction, the compressive strength is high enough to freeze the compressive stress at the interface. As a result, compressive stress has the effect of increasing the Empress restoration resistance to surface damage by opposing the formation of surface cracks. Additionally, the rounded tips of internal microfractures within leucite crystals can limit or prevent fracture progression.3,10 A patented heat-pressed technique was first described in 1936 for the construction of ceramic complete dentures.11 However, a commercially available furnace was never developed. In 1969, Droge described a ceramic press technique based on the hot-press technique. Improving the previous technique, Mc Phee was able to produce complete-coverage metal-ceramic restorations that accurately duplicated occlusal surfaces.11
In 1983 research of a leucite-reinforced glass ceramic was initiated at the University of Zurich by the department of fixed and removable prosthodontics.3,11,12,13 As a result, in 1987 IPS-Empress *Ivoclar, Schaan, Liechtenstein* became commercially available as an attempt to improve the mechanical properties of conventional ceramic materials whist maintaining the benefits of lasting aesthetics and biocompatibility.3,11 The Ivoclar development team not only reached their goal of a greater ultimate strength, but also perfected a system with a simplified method of fabrication.14,15Initial trials indicated that IPS-Empress could become an alternative that is less time consuming and less technique sensitive than other ceramic materials. The new material is a fine-grained high strength pressed glass-ceramic (injection moulded) which has the following composition in wt % : 11
63 % SiO2, 17.7 % A2O3,
11.2 % K2O, 4.6% N2O,
0.6 % B2O3, 0.4 % CeO3,
1.6% CaO,
0.7 % BaO and 0.2 % TiO2.
The high-technology of the Empress system is thorough in conception with perfectly matched components. The entire IPS Empress system is composed of the following materials :3,10,11.16

The ceramic ingots are precerammed and available in the full Vita and Ivoclar (Chromoscop) colour range to more closely approximate the base shade of the desired restoration. They are also available in varying degrees of opacity3,11.

The following advantages have been reported in relation with IPS-Empress system.3,17
In a practical sense, an increase in the strength of restored crowns may be produced by
two methods: 3
It has been proposed that the combination of hydrofluoric acid (HF) etching, silaning and using of a resin-based luting cement may work mechanically and increase the fracture resistance of restored crown.19
Marquis in his study20 concluded that resin-based luting material may reduce the potential for crack propagation by healing surface defects.This property of resin-based luting cements, may compensate the moderate fracture strength nature of different ceramic systems (IPS-Empress) which may increase significantly their strength by composite resin cementation.
Bonding both the cement / ceramic interface and the cement / dentine interface a further increase in strength has been observed in a laboratory study19. The bonded hydrophobic resin composite layer may help exclude water access to the ceramic; hydrolytic degradation being implicated in strength reduction after dynamic fatigue. There are indications that clinical fractures with full ceramics generally initiate at the inner surface, an observation that further supports the reinforcing effect of composite luting agents.19
In relation with the second mechanism of improving fracture resistance, systems with high fracture rate structure, such as the In-Ceram system, may withstand excessive load even if a resin-based cement is not used for the cementation procedure. In this situation, the significantly high fracture resistance of the system is provided mainly from its structure, as highly condensed alumina particles have a reinforced effect.6
Even though the higher strength of newer ceramic systems remains an advantage, reduced failure rates have possibly been influenced more by advances in adhesive cementation materials than by increases in ceramic strength. A reduction in clinical failure rates for full ceramic materials has been reported with adhesive cementation.
In addition, low flexural strengths for cast Dicor *(93.2 MPa) and veneered Dicor (85 MPa) were reported compared with feldspathic veneer porcelain (88.6 MPa)19.
Luthy et al.21 reported similar findings for Dicor but a significant difference in flexural strength for In-Ceram when core (419 MPa) and veneered core specimens (323 MPa) were tested. In another study published by Lehner and Scharer,22 IPS-Empress showed 182MPa flexural strength in comparison with Porcelain Jacket Crown (71 MPa), Dicor (114 MPa) and In-Ceram (419 MPa). Seow et al.23 in their study reported mean flexural strength of 90 MPa, 114 MPa and 578 MPa for Vitadur Alpha, IPS-Empress and In-Ceram respectively. These results would suggest again that In-Ceram restorations are superior to those of Empress and that IPS-Empress restorations do not offer any strength advantage over In-Ceram.
In a study published by Seghi et al.24 different commercially available restorative ceramics were evaluated. In-Ceram and IPS-Empress were unfortunately not included in the test groups. Using a 3-point bending test, flexural strength of the materials has been measured. All of the reinforced dental ceramics (e.g. Dicor, Hi-Ceram) produced mean flexure strength values significantly higher than those of the conventional feldspathic porcelain. However, for more meaningful results, comparing flexural strengths requires several materials to be tested within one study (Fig. 3)
As can be observed from the figure, In-Ceram presents the higher flexural strength in comparison with all the update available ceramic systems. IPS-Empress system demonstrated that subsequent heat-treatment can increase overall flexural strength.
In agreement with this observation is the manufacturer*s report.3,10 Additionally Luthy et al.25 and Gampbell et al.26 in their studies have shown that a significant increase in the flexural strength of Empress can be achieved after simulated heat procedures (simulated veneer firings, surface coloration firings, or glaze firings), as the material's strength values ranging from 160 to 182 MPa. However, both of them report that the basic strength of Empress glass-ceramic has been shown to measure approximately 120 MPa. This value is measured in Empress which has been divested from the muffle but not exposed to further heat treatment or layering.
In agreement with the observations of the previous study is the study of Scherrer and de Rijk28 who compared the flexural strength of In-Ceram, Dicor and feldspathic porcelain crown, using 3 different crown lengths with each material. The crowns were cemented with light-cured resin. For all the materials the fracture load increased with increasing crown length.
In-Ceram showed again the highest flexural strength in comparison with values obtained with feldspathic porcelain and Dicor in all 3 different crown lengths. Another study by Probster and Diehl7 concluded similar results. They compared In-Ceram for which they recorded a crown fracture mean load of (1609 N), with feldspathic porcelain crown (916N) and a metal-ceramic crown (1557 N). As in the previous studies they chose to cement all the specimens using zinc phosphate cement.
Even if the results of the different studies are positive in relation with the development of a high-strength ceramic material, the search never stops.
A number of studies have been published in relation with IPS-Empress (leucite reinforced glass-ceramic) and its comparison with other ceramic systems. Probster8 compared the fracture strength of In-Ceram (964N) with IPS-Empress (750N) and metal-ceramic crowns (1494N). These results would suggest that In-Ceram is superior to IPS-Empress (Fig 4) but this may be misleading. Unfortunately, all the crowns were cemented with zinc-phosphate cement on a Co / Cr master die, which is far removed from the clinical situation. What would have been more appropriate is resin bonded IPS-Empress crowns compared with zinc-phosphate cemented In-Ceram crowns as it has been shown that the fracture resistance of ceramic material may be improved with the use of an adhesive technique (use of resin composite as the luting media).19
Eden et al.29 found that on average etched ceramic crowns bonded using a dual polymerising resin cement, had twice the load resistance of crowns luted with zinc-phosphate cement.
However, a recent research report, published by Grey et al.30 concluded that when Empress crowns were loaded to failure on brass dies, after cementation with two different luting agents (Variolink, Vivadent and De Trey Zinc, DeTrey Dentsply) no significant effect on strength due to the luting material was determined. Probably, the results could be different if a substrate with bonding characteristics similar to the natural tooth surface was used. In agreement with this concept is the study of Fumuscup and Sorensen,31 who found that all-ceramic crowns (IPS-Empress) cemented with resin based cement, produced an improved crown strength. They also had superior marginal fit compared to the metal-ceramic crowns and other ceramic systems cemented with zinc-phosphate cement.
In a related study, Ludwig17 compared the fracture strength of traditional porcelain jacket crown, Dicor and IPS-Empress. Multiple crowns were fabricated and subjected to a 30 degree axial load until fracture occurred. Zinc-phosphate cement was used for the PJC and Dicor and dual-cured resin cement for the cementation of Empress crowns.In both directions of loading, IPS-Empress restorations showed the highest mean fracture values (2180N) in axial loading and (335N) in 30 degree loading in comparison with Dicor (1565N-253N) and PJC (545N-180N) respectively. The porcelain jacket crown showed the lowest values of fracture strength which is in agreement with what we know about the relatively low fracture strength of aluminous porcelain restorations.
Probster in another study,8 reported a mean fracture load for IPS-Empress crowns of 814N in comparison with 1494N for the metal ceramic crowns. (Fig.4).It is obvious from the different studies in relation to the fracture strength of all-ceramic systems, that the values reported are highly variable. This is because the testing of the compressive strength of crowns is not a standard method. Many factors influence the results: preparation design, crown thickness, direction of the applied load and location of load application. Compressive strength studies of crown systems, within their limits, give an idea for the load-bearing capacity in simulated clinical situations.The results of in vitro strength studies may give helpful information for the design of clinical studies, which have to give definite answers.
In a clinical evaluation of Empress inlays after a period of 1.5 years, Krejci et al.15 have mentioned that even though satisfactory clinical results with no failures or bulk fractures were recorded during the observation time, scanning electron microscopy (SEM) showed marginal breakdown and deterioration of the interface between ceramic inlay and a resin-based luting agent .
A study done from Sorensen et al.35 reported that the clinical performance of Empress full-coverage crowns, cemented with a microhybrid cement (Variolink, Vivadent) during a period from 1 to 30 months, were very encouraging as for 75 crowns no fracture, cracking or extrinsic staining was noted.
In contrast with Sorensen*s results, Lehner et al.34 reported 98 % survival rate of Empress restorations luted with a dual cured composite resin-based cement after 18 months in service with a fracture rate of 2.3 %. In agreement with previous studies, Lehner, Studer and Scharer34 proved that IPS-Empress crowns luted with dual-cured composite resin, after they have been etched with hydrofluoric acid and silanized, showed a survival rate of 95 % after 2 years in service. A similar success rate (94%) has also been reported with 78 crowns in a study at the University of Zurich.34 Results of a parallel study with 130 inlays and onlays in posterior teeth are favourable, with a failure rate of only 2 %.32
Abers, van Dijken and Olofson36 compared clinical results of ceramic inlays, cemented with dual-cured composite resin and glass-ionomer luting cement. After a time period of 3 years, they found that the number of fractured ceramic inlays cemented with composite resin media was smaller than for those cemented with glass-ionomer cement.
3. LUTING AGENTS
Ceramics are very brittle and depend on adequate bonding to tooth structure. Resistance to fracture is probably one of the most important factors influencing their durability. This requires adhesive properties of the luting agent and also a high resistance to chemical degradation.Thus, the primary purpose of a luting cement is to aid retention and to provide a seal for fixed prosthetic devices to prepared teeth.
3.1 Acid-base reaction cements
Acid-base reaction cements have widely been used in practice as the luting agent for the cementation of crowns and bridges.16,37 It is reasonable to question the need to replace them as they are apparently safe to use as long lasting luting materials. The reasons these systems have maintained popularity include a long history of clinical success and their adjustable working time. They are also reported to have high impact resistance and high rigidity. However, because of their shortcomings their use is limited nowadays.38
Cements based on zinc oxide are necessarily opaque due to residual powder and may have a very low pH which can lead to pulp irritation.19,39 In addition, they have been found to present significant postoperative sensitivity *presumably due to the acid content of the liquid* and to have increased solubility in water, especially in the first 24 hours after setting.19
Although zinc-phosphate cements have been used for the majority of castings, they are not considered satisfactory luting agents for the cementation of all-ceramic restorations.16,37 This type of cement is extremely brittle, a property which is reflected by a low tensile strength in the order of 5-7 MPa. Therefore, the promised adhesion to tooth structure is relatively short-lived. Its compressive strength may vary in function with powder to liquid ratio, from 40-140 MPa.40
For the success of the cementation procedure, it is important to control the relative thickness of the cement layer, as this factor ensures the proper seating of the ceramic restoration.41 41This is very difficult to achieve as the thickness of the layer is dependent on the procedure adopted. It is also recognised that variations in thickness will affect the load required to fracture the specimens41 . As a result of these potential variations, it is not possible to convert load to failure measurements to absolute failure stresses. Zinc-phosphate cements have the property to occupy the space between tooth structure and ceramic restoration without any adhesive characteristic.42 However, since this was the luting material of choice for about half a century, it may be construed that its physical properties are adequate for their function even though are poorer than those of composite resin luting materials.43
3.2 Glass-ionomer cements
The use of glass-ionomers for the luting of fixed prostheses has rapidly increased in popularity since their introduction 15 years ago. Although glass-ionomer cements showed encouraging properties, such as a bond to the tooth structure, low grade solubility and liberation of fluoride, these are not advocated for cementation of tooth-coloured restorations as clinical experience demonstrated that they were completely inappropriate for this purpose.34 43 The high rate of clinical failures observed was due to insufficient mechanical resistance and poor adhesion to dental hard tissues or restorative material.34 44
Another factor which may further limit the use of glass-ionomer cements as luting agents is their susceptibility to produce sensitivity. Surveys such as the study of Mc Lean et al.45 has confirmed that there is not much to chose between zinc-phosphate cements and glass-ionomer cements with regard to post-operative sensitivity.
In agreement with the previous study, Bebermeyer et al.46 proved also that no significant difference in sensitivity exists between ceramic crowns cemented with zinc-phosphate cement and those cemented with glass-ionomer cements. However, Johnson et al.47 reported higher sensitivity during cementation with zinc phosphate cement than with glass-ionomer cement. The main causes of pulpal sensitivity can be largely overcome by using encapsulated luting cements or by priming of the axial walls of the tooth preparation with a light-curing bonding agent prior to cementation.48 Factors which probably are involved in glass-ionomer produced sensitivity are:49,50,51,52 low powder / liquid ratio associated with increased shrinkage, acidic properties of cement that might irritate the pulp, dehydration of the tooth, development of excessive hydraulic pressure in the dentine tubules, the over filling of the ceramic crown before the seating process, pre-existing pulpitis associated with bacterial contamination, removal of the smear layer and finally a slow rise in pH during material setting. An additional factor which may restrict the use of glass-ionomer cements for the cementation of tooth-coloured restorations is its poor colour matching with the restoration*s shade, probably because of the higher opacity of the cement.
In relation to glass-ionomer strength properties, Klausen et al.53 showed that glass-ionomer cements exceed zinc-phosphate cements not only in compressive strength but also in tensile strength. On the other hand, several studies examined the contribution of glass-ionomer cements, to the fracture resistance of all-ceramic crowns. In a study by Jensen et al.41 when a glass-ionomer luting cement was used to lute a group of dentine-bonded all-ceramic crowns, fracture resistance was lower than that obtained with those luted in position with dentine-bonded agents and a dual-cured composite resin cement.Even if it may be expected that some bonding would have occurred between dentine and the glass-ionomer cement, the fracture resistance of the crown was significantly decreased, when glass-ionomer cement was used as the luting media. Quite recently, a new type of so called hybrid glass-ionomer has appeared in the market. This system is based on 2 types of setting reactions.
An acid-base reaction between the fluoroaluminosilicate glass and the polycarboxilic acid and a free radical polymerisation of the pendent methacrylate groups of the polymer and HEMA (2-hydroxyethylmethacrylate). Although its manufacturer reports significant improvement in relation to solubility, fracture toughness, radiopacity, fluoride release adhesion to dentine and post operative tooth sensitivity, more research is needed to demonstrate material's acceptability over a period of years.
3.3 Resin composites cements
In comparison with conventional luting techniques, a bonded restoration strengthens the prepared tooth. Furthermore, brittle ceramics can withstand occlusal loads in the mouth due to the adhesive luting procedures. This does not require an extremely high reinforced substructure which is necessary in conventionally luted systems.19
Surface interactions between adhesive luting agents and the tooth may be more critical than those for zinc-phosphate cements because many of these materials are purposed to interact chemically and physically with tooth structure. When compared with zinc-phosphate cements, resin luting media have demonstrated less marginal microleakage and greater retention.37
In general, full-coverage ceramic restorations must be cemented using adhesive technology. Their cementation system, built-up between ceramic and the tooth substances of enamel and dentine, is made-up as follows :19
The cementation with adhesive luting agents shows advantages over cementation techniques using non-adhesive luting media. In comparison with traditional luting cements (zinc phosphate cements or glass-ionomer cements) adhesive technology, evidences improved material properties.19
Eden and Kacicz29 found that on average, etched ceramic crown bonded using a dual polymerising resin cement, had twice the load resistance of crowns luted with a zinc phosphate cement.
Successful use of hydrofluoric acid etching for the ceramic bonding surface followed by silanization cannot be omitted. By maintaining all the necessary steps for the adhesive technique, bond strengths can be reached which are comparable or even higher than the strength of the corresponding substrate itself.19 Doering and his colleagues54 reported that resin bonded porcelain crowns were as fracture resistant as unprepared teeth.In contrast to conventional cements, luting composites can show also high a degree of compatibility between the resin cement and the pulp.
The solubility of the exposed resin luting cement is negligibly low in the oral environment and a film thickness of 20-30 *m is obtained.55
Through the adhesive cementation technique, an additional strengthening of the full ceramic restoration and the restored tooth can be obtained. It has been proposed that the fracture strength of standardised all-ceramic crowns in vitro conditions was significantly increased by the use of a composite resin-based luting agent.56
Furthermore, composite resin luting materials by means of their high polishability and tooth translucence, as well as with their shade reproduction can offer significantly better aesthetic results.19,56 Dual-curing formulas can be used for this scope. Light curing enables the material to be finished immediately after the setting of the marginal area. For the self curing formula, none of these guarantee curing in those areas where light enters only in a weaker form such as deeper parts of the preparation.
Although composite resin luting agents play an important role in the success of the adhesive procedure they are often characterised as being inadequately wear resistant.33 The wear rate of luting composites has been shown to be influenced by the type of cement, with the microfilled ones providing more favourable results than hybrid formulas.33
Greater signs of abrasion can also occur by incomplete polymerisation due to oxygen inhibition, resulting in the weakening of the composite system. Oxygen inhibition occurs especially in the surface area of composites, where oxygen concentration is highest. Covering the margins of the restoration with an air blocking agent (glycerine gel), prior to curing can eliminate the primary oxygen inhibition.33
Shrinkage stress after polymerisation, despite the small quantity of luting resin, is another factor which must be taken in consideration. It is conceivable that this polymerisation shrinkage stress compromises the physical properties of the respective material and thereby leads indirectly to increased wear rate.
The inherent shrinkage stress of the luting composite resin, may also be responsible for post-operative sensitivity and cervical marginal discolouration. Shrinkage of even 100 *m of luting media, if the volumetric contraction of the material is 5%, can open a gap of 5 *m which may produce discolouration. In addition, sensitivity may be produced as shrinkage of the luting cement in the horizontal plane may open internal gaps.33 According to the hydrodynamic theory, restoration flexure under occlusal loading compresses this fluid-filled internal gap leading to sensitivity.57
A further reason for the strengthening effect of composite resin-based luting materials has been given from Nathalson58 who indicated that although shrinkage during resin polymerisation is generally viewed as a negative property, within certain limitations the composite resin polymerisation shrinkage may help to strengthen porcelain by exerting a force on the inner porcelain surface that stresses porcelain molecules together rather than away from each other.
3.4 Summary
While much work has been carried out over the previous years to assess the strength of the more traditional dental porcelain materials, not enough information has been reported concerning the relative strength of many of the newer ceramic materials, already introduced into clinical practice.
It has been proposed that the glassy matrix is involved in the failure mechanism as all the ceramic materials are considered to consist substantially of a glassy matrix with various amounts of dispersed crystalline phases and the possible presence of random fabrication defects.3 However, in their article Peterg et al.18 concluded that the crack initiation of ceramic restoration starts at the internal occlusal surface near the pulpo-axial line angle, and externally, near the loading site. It progresses until a complete crack is present between internal and external occlusal surfaces. The fractured phase is invisible from the external site of ceramic restoration and cannot be detected by the clinician. Failure initiation appears to be a result of the growth in number of microcracks in high stress areas, leading to macrocracks. Crack initiation starts as soon as 60% of the loading needed to complete fracture has been reached.18
The question which arises in relation to the strength of the newer ceramic systems is the following:
<< Can the strength of modern ceramic materials such as Empress be increased with the use of composite resin-based as a luting agent ?*>>
In other words, can the combination of an adhesive bond with a relatively low-strength ceramic work synergically to enhance the strength of the tooth-restoration system *
4. PURPOSE OF THE STUDY
The manufacturer of Empress system advises the etching and silane coating of the inner restoration surface and the use of an enamel and dentine bonding system with a dual-polymerising adhesive resin. Therefore, higher strengths can be expected, but a number of problems associated with dentine bonding and the clinical behaviour of resin composite cements are still unresolved.
The aims of this study are:
The objective of this study is to establish if resin-bonded crowns provide a potentially superior performance by measuring their fracture resistance compared with acid / base cemented crowns.
5. MATERIALS AND METHODS
5.1 Sample selection
A total of 36 premolars were collected from the clinics of the Charles Clifford Dental Hospital in Sheffield (UK). All the premolars were cleaned, polished with flour of pumice and evaluated for coronal and root integrity. Only those teeth with fully formed roots, no coronal defects and free from hypoplastic defects and crack lines were placed in the test population. The teeth were measured in two dimensions, mesio-distally and bucco-lingually taking as a measurement point, the height of their contour using a digital micrometer (Mitutoyo Ltd, Japan). The mean mesio-distal dimension of the test population was 7.015*0.369 mm and the mean bucco-lingual dimension was 9.402*0.535 mm. The teeth were divided into 4 equal groups according to mean measurement of mesio-distal width as follows.
Group 1: <7 mm, group 2: 7-7.25 mm, group 3: 7.25-7.50 mm and group 4:> 7.50 mm. After the division of teeth in the above categories, all the premolars were equally redistributed in 3 groups (groups 1, 2, 3) such that each group had an equal size distribution. A further 3 premolars were selected to form the control group. Calculus deposits and residual soft tissue were removed from the root surface of the selected teeth, with a hand scaler (Hu-Friedy, 3A Leimer Germany). Following post-extraction storage in dilution solution, the teeth were stored in distilled water at room temperature.
Each tooth was embedded into an epoxy resin base (Buehler, Metset mounting plastics, Buehler UK) that allowed accurate placement into the testing apparatus. Special care was taken to ensure that each tooth was fixed with its long axis congruent with the loading axis of the testing apparatus. Each of the specimens was mounted, crown uppermost and long axis vertical to within the cemento-enamel junction. A circumferential line was drawn with a prosthetic pencil exactly to the level of CEJ so that accurate placement of each tooth to that level was possible.
The mounted teeth were stored at 100% humidity-distilled water in room temperature approximately 20 Centiigrade for approximately 3 months until the all-ceramic crowns were fabricated.
5.2 Tooth preparation
These series of reductions, resulted in a tapered preparation with a smooth carbide finish and a 90 degree flat shoulder preparation on the margins. All stages were carried out with a high-speed hand piece operating with water coolant. All the preparations had a height of 5.09*0.13 mm, a total diameter of 8.92*0.36 mm in bucco-lingual direction and an occlusal width of 4.61*0.24 mm on average.


Die stone material (Geo-stone, Bayer Dental Products, Germany) was poured carefully into each impression. When the stone completely filled the impression space, the impression was slightly vibrated and placed under pressure in vacuum (Palamat practic, Kulzer, Gemany) for 30 minutes.
When the vacuum programme finished, the die stone models were removed from the vacuum and placed in room temperature for another 30 minutes.
The models were carefully removed from the silicone impressions and 2 coats of a die-spacer liquid (Fit-rite, Chaperlin and Jacob's, UK) were painted on to create space for the luting material. The spacer also helped smooth out any roughness of the preparation. Special care was taken to avoid placing die-spacer solution into the margins of the prepared teeth. All the die-stone models were numbered to respective tooth preparations.
The same procedure was applied for the reproduction of the initial dimensions of each specimen in bucco-lingual direction by using the second impression sectioned in bucco-lingual way. Attention was given to correct reproduction of the preparations margins and to the smooth surface of all the wax patterns. The wax pattern was carefully removed from the prepared tooth structure with rubber-dam (Dental dam, Hygienic corporation USA) and checked visually for any crack lines through the wax or areas of discontinuity in the finishing line.

Each sprue was placed 90 degree to surface of the wax pattern, as shown in the Fig. 8.

Special care was taken, not to intermix different types of wax. Use of sticky wax was completely avoided. The patterns were separated from each other by a distance of approximately 3 mm. A paper ring was then placed over plastic base and the plastic stabilising ring was placed on top. (Fig.9)

The cylinder was covered with material until a level just below the stabilising ring. Immediately afterwards, the stabilising ring was removed from the cylinder and a plastic trim gauge was placed on the top of the cylinder whilst the phosphate-bonded investment material was still soft. The material was left to set completely for approximately one hour. Then the plastic stabilisation ring, the sprue former and the paper ring were carefully removed. A tungsten carbide cutter (type SJT 141, Skillbond UK) was used to remove all the refractory projections on the base of the cylindrical former until a level, smooth base of the refractory was achieved.
Two ingots of the Empress material were used for every ring which contained 3 wax patterns. The ceramic ingots and the plunger were adapted in a special support stand provided by the manufacturer. The temperature in the burn-out furnace was raised to the maximum temperature of 850*C at a rate of 3* / minute.
The refractory mould and the ceramic ingots together with the plunger were held at this temperature for at least 90 minutes for wax burn-out and heat saturation. After a time period of 4.5 hours the heat-treatment procedure and the preparation for the ceramic pressing were completed. Subsequently, the casting ring was transferred from the burn-out furnace to the hot-pressing machine. It should be noted that 1.5 hours before the end of the heating procedure, the compressor and the hot-pressing machine were switched on, until the vacuum pressure of the furnace reached 5 bar. On completion of refractory pre-heating, the ring was ready to be placed in the furnace.
The burn-out furnace was opened carefully and 2 ceramic cylindrical ingots of TC5 dentine shade (10.5 mm in diameter and 7.5 mm in height) were placed in the sprue former hole. The heat saturated alumina plunger was then set in position, into the recess of the ring with its chamfered edge positioned internally.
The furnace was heated automatically starting from the stand-by-temperature of 700*C to the final programmed press-temperature of 1180*C .
After a 20 minutes holding time at this temperature, the pressing procedure was activated. The ceramic ingots had softened sufficiently to be pressed into the mould (0.3 to 0.4MPa).
As a result, the plunger started to inject the molten ceramic into the form of the restoration left by the wax burn-out phase.
Subsequently, the mould was filled with the glass-ceramic material. Once voids were completely filled, plunger maintained the hydrostatic pressure during the entire cooling cycle. The vacuum and heating process were turned off automatically and an acoustic warning signal notified the completion of pressing phase. The chamber of the Empress system was opened and the investment was immediately removed with gentle movements, using an special instrument provided by the manufacturer (clamp holder). The mould was placed carefully on pins seated into a special stand called a honey comb, specially provided by the manufacturer. This type of base allowed the air to circulate evenly around the surface of the refractory mould. Subsequently, the mould was permitted to bench cool to room temperature for 3 hours.

After complete divesting of the ceramic restorations, the sprues were separated from the crowns using a diamond cut off rotary disk (type 126 Skillbond UK) in a high speed of 25.000 rotations/minute. Full-coverage Empress crowns (Ivoclar, Schaan, Liechtenstein) with 1.5 mm occlusal and 1 mm axial thicknesses were fabricated. Each ceramic crown external surface was then ground with normal grit diamonds and finished with ultrafine flat diamond burs. (Fig.11)

Small discrepancies were identified and corrected by spraying a small amount of Occlude on to the prepared tooth surface and grinding those areas of the internal surface of the crowns where Occlude was present.
After successful adjustment of each Empress crown, all the test population teeth were kept in distilled water to avoid desiccation until the moment of crown cementation. 35 full-coverage Empress crowns were fabricated following the manufacturer's instructions for waxing, sprueing, investing, pressing, divesting, polishing and finishing. Prior to the cementing procedure, the fit of the ceramic crowns on the tooth structures was again examined thoroughly.
5.4 Crown cementation procedure
The teeth were prepared for cementation by thorough rinsing and drying. A universal bonding system was selected in association with 3 different types of luting media (zinc-phosphate cement, glass-ionomer cement and dual-cured composite resin material). Twelve crowns were cemented with each type of the above luting agents. (Table1)
a) Empress restoration pre-treatment: Each Empress full-coverage crown was cleaned with water and dried thoroughly with water-and oil-free air. The inner surfaces of ceramic crowns were etched with hydrofluoric acid 4.9 % (IPS Ceramic etching gel) for 90 seconds following manufacturer's recommendations. The gel was rinsed off and each restoration was dried with water and oil-free air. Neutralisation powder provided by the manufacturer was used to neutralise the hydrofluoric acid and this was collected in a plastic cup.
The inner surfaces of the restorations were silanized with a silane-based one component bonding agent (Monobond-S, Vivadent). Monobond-S was applied with a brush and was left to set for 60 seconds. After that, each restoration was cleaned with water and dried with a water and oil-free air. A thin layer of an unfilled resin (Heliobond, Vivadent) was applied with a brush on the etched and silanized ceramic surface. Excess Heliobond was blown off with water and oil-free air, until a thin layer of Heliobond was obtained. In this way, the wetting of the etched and silanized ceramic surface was improved. To prevent premature setting of Heliobond, the crowns were stored in the special kit provided by the manufacturer until the moment of cementation.
b) Dentine surface pre-treatment: the prepared dentinal surface was cleaned with flour of pumice on a rubber prophylactic cup at slow speed, rinsed with an air-water syringe for 30 seconds and dried with an air syringe for 10 seconds. Phosphoric acid (37 %) was applied to dentine for 1 minute. After that, it was rinsed thoroughly with water and dried with an oil and water-free spray until a frosty appearance occurred on the dentine.
A primer solution (Syntac, Vivadent Schann, Liechtenstein) was applied with a disposable brush on the dentine and was left to react for 15 seconds, until the dentine was of a glossy appearance. Consequently the primer was dried with water and an oil-free air spray. As a result, a layer was formed between the dentine surface and the Syntac solution. Syntac adhesive was applied with a brush on the dentine and left to react for 10 seconds. After that time, it was dried with water and oil-free air. An unfilled resin (Heliobond Vivadent) was applied with a brush on the dentine surface as a bonding and wetting agent. Any excess was removed by a slight air-blow and the material was light cured (Euromax, De Trey Dentsply) for 10 seconds. The microhybrid resin luting cement-Variolink which is presented in two tubes (base and catalyst) was mixed carefully with a spatula in a 1:1 ratio on a mixing block for 10 seconds. Mixed Variolink was applied with a spatula on the fitting surface of each crown and on the dentine preparation area to avoid trapping air.
c) Seating of Empress crowns: Each Empress crown was perfectly placed to the prepared dentine surface with a gentle, minimum finger pressure to reproduce clinical cementation. Any excess luting material was removed with a brush. Finger pressure was increased temporarily and each crown was maintained under pressure for 15 seconds.Residual excess Variolink was again removed with a brush and dental floss (proximal regions). After insertion of the crowns, Variolink was polymerised step by step. Light curing was completed for 60 seconds for each site of the ceramic crown (mesial, distal, lingual and buccal) starting first from the proximal margins.
To compensate for any oxygen inhibition, restoration margins were covered with a neutral glycerine gel (Liquid Strip, Vivadent) after removal of excess luting agent but before polymerisation.
d) Finishing and polishing procedure: When polymerisation of the luting resin was completed, polymerised excess material was removed with superfine finishing diamonds and with flexible polishing disks (Soflex, 3M).
Polishing of restorations margins was done with silicone polishers. Variolink resin is a highly viscous luting composite which, because of its high viscosity, cannot flow out of the preparation area causing marginal deficiencies.
5.5 Fracture testing procedure and strength measurement
Each specimen was orientated in its epoxy resin cylinder base and placed into a universal testing machine (Lloyd instruments Ltd, UK) and subjected to compressive loading with a crosshead speed of 0.5 mm / min. Special care was taken to assure that the compressive force would was directed down the long axis of each specimen. This compressive force was applied by a stainless-steel ball placed along the midline
fissure of each premolar Empress crown so that forces were shared by the triangular ridges of both the facial and lingual cusps. (Fig.12 )

The crosshead speed of the testing machine was stopped when the very first discontinuity of the chart recording appeared as a result of an early crack catastrophic failure (explosive manner). Failure load of each Empress crown was recorded in Newton (N) as well as the location and morphology of the fracture. (Fig.13)

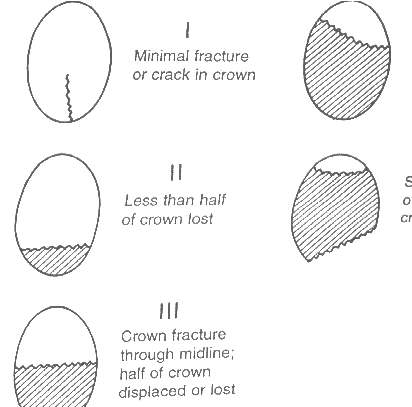
Not all IPS-Empress crowns exhibited a complete fracture of the ceramic. However, because most of the specimens failed in an explosive manner, it should be realised that the fracture images shown, are reconstruction of the crowns from the shattered fragments.



From all the test population, only 2 crowns (one from group 2 and one from group 3) showed severe fracture of crown and tooth. Cracks were visible through the entire thickness of these units and they shattered macroscopically into at least 2 to 3 pieces. (Fig.19)


Thereafter, crack initiation was easily induced at the entire thickness of the sample because of the intrinsic fragility of the ceramic material. until a complete fracture was presented. Crack flaws propagation showed also an extension to the luting cement used for each group. As the fracture failure progressed through the ceramic structure, hackle fracture features, resulting from the fracture process, were microscopic.
Identified hackles (or river patterns) are oriented parallel to the direction of crack advance. These hackles can be visually followed back to the location of the crack-initiation site.(Fig.21)

Examining the fracture mode of Empress crowns in relation to the luting material used for each group, it can be concluded that group 3 showed the least variable ways of fracture as in most of the samples, fracture failure was minimal or less than half of crown was lost. On the other hand, group 1 showed the most variable fracture modes. Different studies59,60 have shown the existence of four distinct regions surrounding the failure initiation site*primary flaw*in ceramics. *1* the mirror region *2* the mist region *3* the hackle region and *4* the macroscopic crack branching region. In this study, not all the fracture regions were easily identified, as the magnification used was not high enough to reveal mirror and mist regions.
An effort was made to identify any possible relation between fracture loads registered and mean dimensions of the prepared teeth and fabricated Empress crowns. The study concluded that no relation existed between the prepared tooth structure or crown dimensions with the obtained fracture load for all the test groups (Fig.22 ).
Clinical implications: Post-testing measurement of the thickness of the crowns at the occlusal fissure indicated that although the study was designed to elucidate the factors involved in resistance to fracture using simulated clinical techniques whenever possible, it was not possible to simulate the conditions under which tooth fracture may occur in vivo. Occlusion plays a primary role in determining the phenomena of static fatigue which causes the propagation of cracks in all-ceramic crowns. In vivo, magnitude or location of masticatory loads and occlusal status differ from the situation in vitro, unless a variety of occlusal loading is included in vitro analyses, because the orientation of the load has an important effect on the development of the stresses. Furthermore, existence of a complex biological environment in vivo, is difficult to reproduce in in vitro studies, and, too often, the crown*s environment in vitro is oversimplified. On the other hand, testing of the compressive strength of all-ceramic crowns is not a standard method.
Several factors influence the results:
a) shape of restoration
b) microstructural inhomogenities
c) residual stresses and stress gradients, induced by polishing or thermal processing
d) thickness variation of the ceramic restoration
e) direction and location of load application.8
The possible interactions among these variables complicate the interpretation of failure analysis observations. The study revealed, by optical microscopy, a variety of fracture surface markings that characterise the fracture origin and the propagation path of the primary crack. In the majority of cases, the crown fractured before tooth substance was damaged; it therefore appears that, while the dentinal bonding procedure may enhance fracture resistance of all-ceramic crowns, an adhesive luting technique is not necessarily required to protect underlying tooth structure from fracture. The fracture markings act as a detailed record of the fracture process. Probably an SEM fracture analysis was also necessary because of its superior depth of field when compared with optical microscopy and because of its ability to resolve features with dimensions less than 1 *m. Not enough information is available to date in relation to the mode of fracture of Empress crowns clinically. A manufacturer*s study reported that the Empress crown cemented with a resin-based dual cement, demonstrated a fracture though the deep, central fissure which was not visible clinically, but discovered during an SEM examination.33 This observation is in agreement with the fracture mode results of the third group crowns of this study as the majority of crowns presented a minimal fracture line through the midline, without any loss of crown. Of course, further research is needed clinically.
The standardised method of application of force, may allow comparison to be made between the different luting procedures utilised and the control group. Besides, fracture strength values of Empress crowns within their limits, give an idea for the load-bearing capacity of this new ceramic material. The results of the study may give helpful information for the cementation procedures of Empress crowns in clinical situations. As the mean maximum chewing forces between 2 antagonists in humans range between 245 N and 540 N 8 it may be stated that IPS-Empress crowns have sufficient strength to allow clinical testing.
The mean fracture load value for the Empress crowns cemented with three different procedures cannot be related to the values of previously reported studies8,17,30 for Empress glass-ceramic, as different substructures were used compared with this study. Certain difficulties have been faced with the satisfactory production of Empress crowns.
The fabrication technique proposed by the manufacturer was found to be time consuming and quite sensitive.The production of an accurate fitting crown surface was very difficult as it depended on the existence or not of air bubbles in the refractory material. Pouring of the refractory into the mould needed special care. It was found critical to fill perfectly the internal surface of each crown wax pattern with refractory material.
When this condition was not respected, a repeat of the fabrication cycle was necessary. Difficulties were also faced in relation to the proper adaptation of Empress crowns onto the prepared dentine surfaces. Existence of apparently insignificant undercuts in the prepared tooth area made the correct adaptation of the crowns impossible. Identification of small undercuts was difficult as the wax patterns, because of their plasticity, were easily removed. In these cases, observation of the preparations under a microscope was necessary.
Another interesting observation in the study was related to leaving the wax patterns inside the refractory mould for more than 24 hours, a fact which had a significant result on the external aspect of Empress crowns after pressing and divesting procedures. Empress crowns in this situation appeared full of porosities and irregularities.(Fig.23 )A repeat of the fabrication procedure was necessary.

Enough attention must be given also to all the equipment used for the Empress fabrication cycle. All the devices used must be controlled carefully before their use. During the study, an obstruction in the vacuum system, during the mixing stage of the refractory material, caused irreversible damage to the final Empress crowns.A number of previous studies on intracoronal restorations have indicated that the use of bonding techniques may provide enhanced resistance to fracture.62,63,64 In contrast, Stampalia et al.65 indicated that the use of a resin-bonded ceramic does not increase the fracture resistance of teeth.
In another study, Mc Cormick et al.66 reported that all-ceramic crowns luted with zinc phosphate, glass-ionomer and composite resin cements did not shown any statistically significant difference among fracture strengths. However, in that study a dentinal bonding agent was not used in conjunction with the resin composite lusting material, a factor which may explain the apparent divergence between the results obtained by McCormick66 and those obtained in the present study.
The group of Empress crowns which were luted with a non-adhesive luting material, showed the lowest fracture resistance. This may be due to the lack of bonding, given that it has been reported that such a cement merely occupies space without offering any adhesive property.42 Additionally, its physical properties are poorer than those of resin-based luting materials.43
In relation with the other traditional luting material used in the present study, results obtained are in complete agreement with previous studies. Jensen et al. 41 concluded that glass-ionomer cements used to lute dentinal bonding all-ceramic crowns have lower fracture resistance than those obtained with dentinal bonding agents combined with a dual curing composite resin cement.
Although some bonding can be achieved between dentine surface and glass-ionomer cement, it is not possible for the glass-ionomer to withstand the applied loads successfully.
The results of the present study indicated that the use of dentinal bonding in conjunction with a resin-based composite luting material provided resistance to fracture that was not significantly superior to that obtained when no dentinal bonding was used, as no important statistical difference was identified.
This concept is contrary to the results of previous studies.63,64,65 However, the apparent higher fracture resistance of ceramic crowns bonded with a resin-based cement may be due to:
A higher fracture resistance was expected from third group of samples cemented with a
resin-based luting material. Probably, if all of the heat treatment cycle of the Empress
crown was followed (simulated veneer firings, surface coloration firings, or glaze
firings), the fracture resistance values obtained could be different. As a result, it is
suggested that further studies are carried out to re-evaluate the fracture resistance of all-
ceramic crown when all the fabrication stages have been completed fully.
8. CONCLUSIONS
The effect of the luting cement on the fracture strength of all-ceramic crowns of
Empress material was evaluated. Within the limitations of the study design, the
following statements may be made:
1. A luting procedure that includes dental bonding in conjunction with a composite resin-based luting material and an etched ceramic fitting surface provides a relatively higher fracture resistance in all-ceramic crowns (IPS-Empress) compared to similar crowns luted with a glass-ionomer or a zinc phosphate cement.
2. In the group of test samples in which dentinal bonding procedure was omitted (groups 1 and 2), resistance to fracture was less than that found in group 3 in which bonding procedure was applied.
It would therefore appear that the resin-based luting material plays an important role in improving fracture resistance, either by its physical properties or by prevention of crack propagation
However, no statistically significant difference in the fracture strengths of bonded Empress crowns and those luted with conventional luting cements was found.
Other factors, such as marginal integrity, require assessment. In addition, further clinical trials are required to assess the potential of the dentine bonded ceramic restoration.
![]()