Browse through our Journals...
The Psychiatric Rehabilitation and Evaluation Program (PREP): A Clinically Effective Model of Treatment for Persons with Severe and Persistent Mental Illness
O.J. Oluboka, M. Saltstone, S. Stewart, D. Brown-Demarco, S. Deschenes, D. Wallace and Susan Adams
Northeast Mental Health Centre, North Bay Campus
Abstract
This paper will describe the development of an interdisciplinary regional tertiary mental health service located in an under-serviced area of Northeastern Ontario, Canada. The results of clinical program evaluation indicators will also be presented, highlighting the clinical effectiveness of the program model. Specifically, clinical data collected to date demonstrate reduction in readmission rates, functional improvement and symptomatic recovery in patients admitted to the program. Significant predictors of readmission to hospital include whether the full PREP program was completed and number of previous hospitalizations. The success of the PREP model suggests that a combination of inpatient/outreach services, a cohesive interdisciplinary team, use of videoconferencing and teleconferencing technologies and evidence based evaluation measures collectively contribute to maximum clinical effectiveness.
Introduction
As part of the Ontario provincial government’s attempt to downsize psychiatric hospitals, the Health Services Restructuring Commission recommended the divestment of regional specialized psychiatric services based at the North Bay Psychiatric Hospital (North Bay, Ontario, Canada) to the Northeast Mental Health Centre, and the acute care district services to the local general hospital (North Bay General Hospital, North Bay, Ontario, Canada). As a result of this directive, it became apparent that the two services needed to be clearly delineated. This served as the primary impetus for the formation of the Psychiatric Rehabilitation and Evaluation Program (PREP). One of the principal objectives of efforts to reform the mental health care system is to improve care for individuals suffering with severe and persistent mental illnesses (SPMI) (Wasylenki et al., 2000). Strategies implemented to date involve increased resources for community supports and services to reduce reliance on hospital-based services (Ontario Ministry of Health, 1999). These strategies, which have included case management, assertive community treatment, appropriate housing, shared-care and medication compliance initiatives, are able to meet the needs of most individuals suffering with SMPI (Chamberlain & Rapp, 1991; Holloway, 1991; McGrew, & Bond, 1995; Solomon, Draine, & Delaney, 1995; Thompson, Griffity, & Leaf, 1990; Thornicroft, 1991). However, there are subgroups of patients who cannot be managed by either primary or secondary services. These patients require more sophisticated assessment and/or management, which may in turn indicate a need for other forms of specialized tertiary care (Bigelow et al., 1988; Trieman & Leff, 1996; Gudeman & Shore, 1984).
Mental Health reform principles and implementation strategies both underscore the need to clearly delineate levels of service along primary, secondary and specialized tertiary care dimensions. There is also a need to differentiate district (local) first line services from specialized regional (centralized) services in order to ensure an equitable distribution of services and resources to patients from all areas regardless of proximity to the central site. With the increasing complexity of mental health service delivery systems comes an increased need for collaboration and integration at all levels to provide adequate and comprehensive care for persons with SPMI in the community.
The Psychiatric Rehabilitation and Evaluation Program (PREP) is a unique and innovative interdisciplinary team care approach which was designed to provide mental health treatment to individuals living in under-serviced regions of Northeastern Ontario, Canada. Under the hospices of the stated goals of mental health reform and based on best practices, PREP was envisioned to be an integral and complementary part of a regional mental health care delivery system (Figure 1).
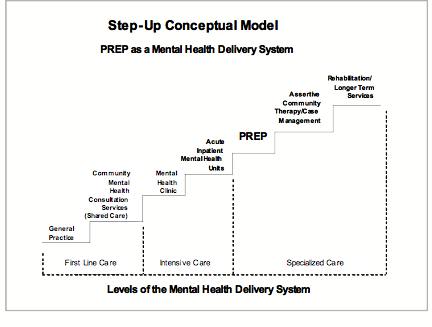
Figure 1: Conceptual model of the comprehensive service continuum where PREP is the first step into tertiary or specialized level of patient care
The Northeastern region of Ontario (figure 2) covers a vast geographic area of 300,000 square kilometers with a population that just exceeds 700,000 inhabitants. Environmental, economic, cultural and social factors have a tremendous impact on how mental health treatment is delivered. The immense size of the region coupled with its sparse population density and numerous remote and isolated communities requires special attention. Significant distances between health care centers with core treatment services are a limiting factor in ensuring availability and timely access to these services. Harsh climatic conditions and difficulties associated with transportation problems impact both service delivery and health status. Health status indicators suggest a higher prevalence and incidence of mental illness as a result of these conditions. Social factors such as education, income and employment are recognized as key factors affecting the health status of any general population. Relative to the rest of the province, this particular region is characterized by lower educational attainment levels, lower family incomes, higher rates of unemployment, higher rates of substance use and higher morbidity and mortality rates. Due to low population density, public transportation including airplanes, trains and busses are operated at minimum levels creating further barriers to accessing mental health treatment. Travel is very time consuming and expensive for both individual clients and service providers. Culturally, the special needs of Francophone and Aboriginal people must be taken into consideration when determining the composition and location of mental health services.
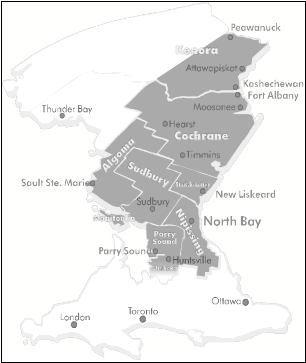
Figure 2: Extent of the geographic area for which PREP provides specialized mental health services (approximately 300,000 sq. km)
The primary target population of PREP is individuals identified to be suffering with complex and refractory mental health disorders. A variety of interventions, ranging from community consultation, telehealth technologies, time limited inpatient evaluation and customized care plan initiation are integral components of the program. In order to demonstrate the clinical effectiveness of any program or treatment, objective, quantified evaluation should be conducted (Andrews & Whittchen, 1995). Accordingly, PREP incorporated standardized evaluation instruments using the strategy of repeated measurement in order to objectively assess changes in the clinical status of patients over time. Evaluation measures included standardized ratings of severity of illness, symptom ratings, functional and symptomatic improvement indicators and medication profiles. Demographic variables (i.e., age, gender, marital status, community of origin), individual difference variables (i.e., number of previous admissions, length of stay in hospital, clinical diagnoses) and whether patients completed the full PREP program were also monitored.
In essence, PREP was designed with the ultimate goal of improving the quality of service and support for patients with SMPI in remote areas of Northeastern Ontario, Canada in order to ensure that patients with SPMI would optimize their independence, successfully reintegrate into their home communities and maximize their overall quality of life. It was hoped that PREP would be a “bridge” between local district services, the community and other specialized programs of the Northeast Mental Health Centre. Patients with complex and treatment refractory problems would be treated in the least restrictive environment possible in order to prevent long-term hospital admissions and achieve the stated goals of PREP.
Method
Procedure
PREP was designed to be an entry point transition to other specialized mental health services available at the Northeast Mental Health Centre. Incorporating inpatient, outpatient and outreach services, PREP served as both a mental health service and mental health delivery system (Figure 3). PREP accepted referrals from community psychiatrists, Schedule 1 facility psychiatrists, ACT teams and tertiary care psychiatrists. Each referral was reviewed by an interdisciplinary team and prioritized based on level of intervention required (Figure 4).
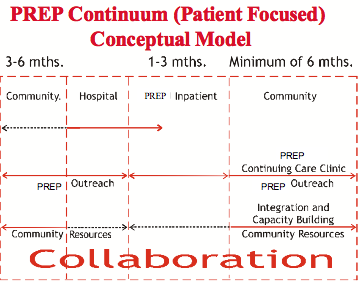
Figure 3 Model of patient focused collaboration with PREP and community
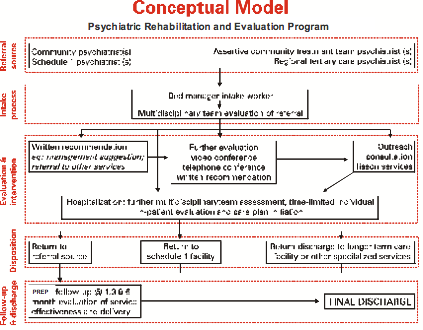
Figure 4 The processes of the PREP model from referral to discharge
The interdisciplinary team included a psychiatrist, several clinical nursing staff, a nurse manager, an outreach coordinator, one psychometrist, two social workers, one concurrent disorders clinician, one recreational therapist and one occupational therapist. This enabled the provision of comprehensive multidisciplinary assessments, investigations and clinical interventions. A global bio-psychosocial-spiritual approach was implemented, with due sensitivity to culture and its impact on patients psychopathology.
All patients admitted to the program provided consent for any data collected on them to be used for evaluation, research and publication purposes. The method of data collection was naturalistic with no blinding of clinicians and patients. Completion of the standardized evaluation tools provided the primary source of data used to assess the effectiveness of PREP. Ratings on each patient were collected at intake and discharge, with some measures completed more frequently to allow for comparison of symptoms and treatment evaluation. All data was analyzed using SPSS for Windows 10 ("SPSS For Windows," 1999).
Clinical Measures The following scales were used to rate patients’ symptoms and behaviours in order to track changes during their admission to the program.
-
The psychiatrist rated all patients on Severity of Illness (where “0” represents “no assessment” and “7” is “among the most extremely ill patients”) and Global Improvement (where “0” is “no assessment” and “7” is “very much worse”) using the Clinical Global Impression (CGI) scale (U.S. Department of Health, Education and Welfare, 1976).
-
The Global Assessment Scale (GAS) (Endicott, Spitzer, Fleiss & Cohen, 1976) was used by the psychiatrist and other clinical staff to rate current level of functioning on a hypothetical 10 point continuum of mental health-illness (where “91-100” represents “no symptoms and superior functioning” and “1-10” indicates that the patient requires “constant supervision to prevent hurting self or others and no attempt to maintain personal hygiene”).
-
The BASIS-32 (Behaviour and Symptom Identification Scale) (Eisen, Dill & Grob, 1994) is comprised of a 32 item 5 point Likert scale (where “0” represents “no difficulty” and “4” reflects “extreme difficulty”) that each patient completed. Items assess a variety of symptoms and behaviours, such as “adjusting to major life stresses” or “mood swings and unstable moods”. A high score reflects more severe behaviours and symptoms.
-
The Brief Psychiatric Rating Scale (BPRS) (Overall & Gorham, 1962) is an 18 item 7 point Likert scale (where “0” represents “not assessed” and “7” represents “extremely severe”) which was completed by nursing staff in order to evaluate a patient’s psychiatric symptomatology. Items include specific symptoms such as anxiety, tension, grandiosity, hallucinatory behaviour and disorientation, with a high score reflective of more severe symptoms.
Results
Patient Demographics: One hundred and twenty four patients were admitted to PREP between 2001 and 2005: 30 patients (24.2%) in 2001/2002; 36 patients (29%) in 2002/2003; 30 patients (24.2%) in 2003/2004 and 28 patients (22.6%) in 2004/2005. There were no significant differences in demographic variables (sex, age, ethnicity, etc.) between patient cohorts over those four years. The age range of the patients spanned from 18 years to 72 years of age (M=37.31, SD 13.05). Fifty two percent of the patients were male. Only about 10.5% of the patients had achieved a college or university degree. Most patients had attended high school but did not graduate (49.2%). Ten and one-half percent had achieved a grade 8 education or less. Most patients had never been married (65%); about 14% were married at the time of admission and 21% were separated, divorced or widowed. Patient income was generated primarily through government sources and/or family (91%).
PREP Catchment area: Patients were admitted to the PREP program from a variety of referring sources. Approximately 2% of patients were admitted from the Muskoka/Parry Sound district (population 92,772); 16% from Timiskaming (population 34,442); 18% from Sudbury/Manitoulin (population 190, 841); 18% from Sault Ste Marie/Algoma (population 118,567); 22% from Cochrane (population 85,247) and 23% from Nipissing (population 82,910). Only one patient was accepted into the program from outside the catchment area. While the greatest percentage of patients were admitted from the Nipissing district, per capita data suggests that the Temiskaming district was the origin of most patients with an average of 14.52 per 100,000 (Figure 5). Annually, the PREP program admitted 5.08 patients per 100,000 of the general population from the northeast districts (Statistics Canada, 2001).
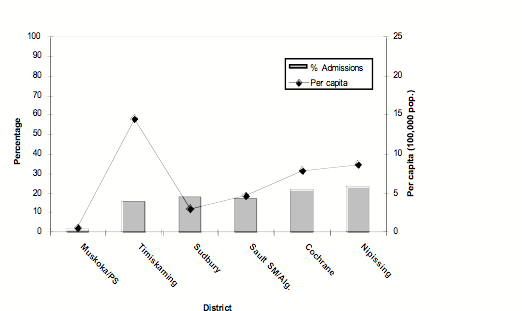
Figure 5 Comparison of the percentage of admissions from each district of origin from 2001 to 2005 to the number of admissions per capita (100,000 population) per year to the PREP program
Trends: Admissions and Length of Stay:
The average number of days spent in the PREP program was 93.3 days, with the range spanning 1 to 306 days (SD 56.26). Patients admitted to the PREP program had an average of 10.83 previous hospital admissions. Some general trends were 1) the older the patient when admitted to PREP, the higher the number of previous admissions to hospital (r =.22, P<.05); 2) the older the patient the more severe the rating of severity of illness (r =.24, P<.01; Severity of Illness and CGI); 3) the more severe the rating of illness at intake, the more likely the patient would require a longer PREP admission (r =.28, P<.01).
Patient Diagnoses: Most patients who were admitted to PREP were diagnosed with a psychotic or mood disorder. Using DSM-IV-TR categorizations (American Psychiatric Association, 2000) on Axis I, 48% of patients were diagnosed with Schizophrenia, 13% with Major Depressive Disorder, 12% with Bipolar Disorder and 11% with Schizoaffective Disorder. Approximately 5% were diagnosed with substance related disorders, including substance induced psychosis. On Axis II, personality disorders accounted for about 34% of all diagnoses, with 11% of those cases diagnosed with Borderline Personality Disorder. About 10% of the patients were diagnosed with Mental Retardation. Approximately 69% of the patients were assigned differential or co-morbid diagnoses. In terms of co-morbid medical conditions listed on Axis III, 11% were diabetic, 6% had hypothyroidism, 5% had Hepatitis C, 3.2% were obese, 2.4% were incontinent and 2.4% had heart disease. It is evident that patients admitted to the PREP program present with chronic and complex symptomatology within the psychiatric and general medical dimensions.
Medication Issues: Trends Medications were usually prescribed to the patients on the PREP program given that approximately 50% of them were diagnosed with Schizophrenia and about 25% were diagnosed with Bipolar Disorder. Overall, typical antipsychotics (i.e., loxapine, depot flupenthixol, flepenthixol, haloperidol, and chlorpromazine) were rarely prescribed as only about 16% of the patients were identified as needing these types of medications. This is in contrast to the novel antipsychotics (i.e., Seroquel, risperidone-depot and oral, clozapine, olanzapine) which were prescribed for approximately 83% of the patients (see Figure 6). Preference for prescribing novel antipsychotic medication changed over time. For example, use of olanzapine fell from a rate of 56% of patients requiring antipsychotics in 2001/2002 to only 8.6% of patients requiring antipsychotic medication in 2004/2005. Risperidone (depot) and Seroquel were the most prescribed medications in 2004/2005 (30% of patients) followed by risperidone (oral). If a second antipsychotic medication was required for stabilization in 2001/2002, olanzapine was almost always used (59% of patients) followed by risperidone (33% of patients). By 2004/2005, the most prescribed adjunct antipsychotic was Seroquel (67% of patients) followed by risperidone (33 % of patients). Lithium has been increasingly prescribed in the program (from 8% of patients in 2001/2002 to 43% of patients in 2004/2005) as a mood stabilizer compared to divalproex (50% of patients in 2001/2002 to 18% of patients in 2004/2005). Wellbutrin SR (32% of patients with depression) and Celexa (26% of depressed patients) was the primary antidepressant prescribed. Clonazepam (59% of patients requiring hypnotic medication) and trazadone (27% of patients) were the most frequently prescribed hypnotics.

Figure 6: Changes in types of novel antipsychotic medications prescribed for patients requiring antipsychotic medication from 2001/2002 to 2004/2005.
Medication Issues: Reduction: Figure 7 illustrates medication changes (in terms of number of medications) from admission to discharge. Individualized psychiatric treatment includes ensuring that each patient’s symptoms are reduced so that the patient is sufficiently stable to allow for a successful transition to their home community upon discharge. Patients were typically referred to PREP following an acute decompensation of their illness and were formerly chronic users of community resources. These attributes are in part a result of the use of standard treatment models for administering psychotropic medications to the general psychiatric population. Admission into PREP allowed for strict treatment under the care and observation of a psychiatrist in order to determine the best possible combination of psychotropic medications. Figure 7 shows that significantly fewer medications (and medication combinations) were required to stabilize the patients at discharge (t [121] = 4.905, P<.0001). This is most likely due to the ability of PREP to individualize treatment and closely monitor patient response to medication changes.
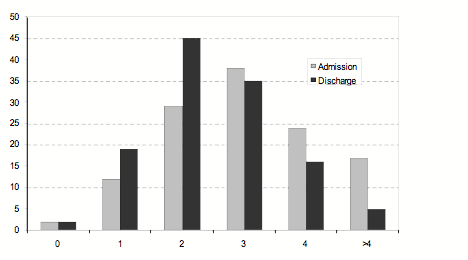
Figure 7: Changes in the number of psychotropic medications from PREP admission to discharge
Patient Improvement: All patients were rated on various scales at both admission and discharge, thus allowing for changes in global health status to be quantified. The mean GAS discharge rating (Mean=61.46) was significantly higher than the mean GAS admission rating (Mean=26.59) (t [122] = -19.862, P<.001), indicating an improved level of functioning at discharge. The CGI scale scores also indicated significant patient improvement by discharge (Mean = 1.88) compared to the initial ratings of severity of illness (Mean = 5.46; t [122] =30.679, P<.001). On the BPRS, the patients lower total scores at discharge (Mean=33.12) indicated significant improvement compared to admission scores (Mean =54.98; t [120] =15.265, P<.001). Significant improvement was noted on all items of the BPRS. The BASIS-32 total score at discharge (Mean=28.11) was significantly lower than at admission (Mean=60.83; t [102] =13.245; P <.001), suggesting that patient self-assessments were congruent with staff assessments.
Readmissions: While there were only seven patients readmitted to the PREP program since 2001, earning the program a success rate of 91.9%, 29 patients (23.4%) were readmitted to hospital within 18 months of their discharge. Ten (34.5%) of those readmitted to hospital were diagnosed with Schizophrenia and five were diagnosed with Schizoaffective Disorder (17.2%). Twenty (69%) of the readmissions had a secondary diagnosis on Axis I and 13 (44.8%) of the patients also had a diagnosis of personality disorder on Axis II. This illustrates the complexity of the symptomatology of these individuals and is perhaps related to the necessity for readmission.
Predictors of Successful Outcome: Several variables collected by PREP were predictive of patient disposition and/or successful outcome. The following predictors were statistically significant but modest (accounting for 9%-12% of the variance in the dependent variables):
-
Level of education and severity of illness (measured by the CGI) was predictive of the number of days the patients spends in hospital as a PREP participant, with the higher the level of education achieved and the more severely ill the patient, the longer the time spent on the program.
-
The shorter the patient’s admission and the less their symptoms improved during that time, the more likely the patient was to have prematurely exited the program without completing their individualized treatment plan.
-
Patients who did not complete their treatment plans and who had many previous hospitalizations, were more likely to be readmitted to hospital after discharge.
Discussion
Although patients admitted to PREP were from varied backgrounds with complex diagnostic presentations, demographic variables appeared to make little difference to an individual’s ultimate success in the program. This relatively new format of treatment delivery was able to demonstrate that patients with SMPI were able to significantly improve over the course of PREP treatment. It was demonstrated that those individuals who remained for a lengthier period of time in the program and completed their individualized treatment plans were less likely to be readmitted to hospital. At discharge, PREP participants required fewer medications to achieve psychiatric stabilization compared to those prescribed prior to admission, especially if the patient was initially prescribed more than three medications. Preference for different types of prescribed medication and medication combinations for patients changed over the course of four years. For example, Risperidone (consta) and Seroquel were the novel antipsychotic medications of choice in 2004/2005 replacing onlanzapine as the most frequently prescribed medication in the first year of the program. These changes highlight the dynamics of the PREP program in that by recognizing the individuality of each patient and the complexity of presenting symptoms, the PREP team is able to discover what “works” in terms of enhancing positive outcomes.
The program’s ability to change and adapt and continue to provide successful care to individuals despite gender, age, ethnic background or complication of diagnoses, further supports the model of “specific treatment” for the “specific individual” both in hospital and subsequently into their home community.
Measurement is essential in order to continue to examine the success of the program and also to effect changes leading to continual program improvement. While predictors discussed in this paper were statistically significant, they did not account for a great deal of the variance in the criterion of readmission. Some of the measures collected to date were found to be so closely related that they were almost duplications, while there were several areas where additional information would be more useful in evaluating the program. For example, there was no information available from community partners that would address what specific factors led to patients being readmitted to hospital (i.e., patient stops medication, patient develops another medical problem, patient discontinues PREP treatment plan, etc.). Additionally, this paper focused primarily on the medication aspect of treatment and paid little formal attention to the contribution of the entire multidisciplinary treatment team. The dedicated work of the entire team in providing therapy, counseling, education and planned physical fitness activities with all patients obviously cannot be overlooked as contributing to overall patient improvement. While generally acknowledged that along with medication, patient groups, education and other treatments offered within the PREP program “canopy” work together to maximize patient wellness, there were no specific measures collected to determine the extent to which the latter are directly related to patient improvement.
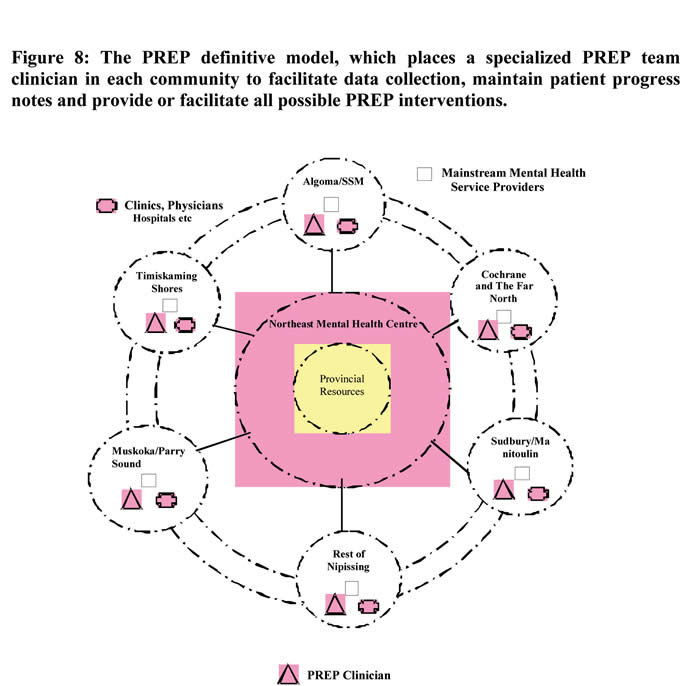
Through the implementation of the PREP “definitive” or “ideal” model of service, data collection within each referring community would be facilitated, as would the ability to inform the continuing progress of patients (see Figure 8). The goal of this definitive model is to expand the PREP treatment team to include a specialized mental health clinician in each of the Northeastern Ontario communities falling within the catchment area. The quality and quantity of outpatient services is likely to improve as the clinician would provide, or facilitate, all possible PREP interventions, such as community consultation, primary health care provider clinical skill development, education, community mental health capacity building, time limited inpatient evaluation and care plan initiation. As a resident of the patient’s home community, the clinician would also be able to provide clinical services, support to existing mental health services and act as a “bridge” providing assistance with transition and integration for patients upon returning to their home community. Obtaining new program measures and readmission related data are future goals of PREP.
Finally, since the PREP treatment team is committed to high standards with respect to understanding needs, communication and education, not only with patients but with families and community partners, team members continue to consult with stakeholders regarding the ongoing development of service quality and satisfaction measures.
In conclusion, the development of PREP was a “breakthrough” in its design. PREP is a mental health delivery system that complements existing mental health models and is able to successfully serve a very large catchment area in Northeastern Ontario, Canada. Quality and effectiveness in patient care and service delivery to include remote areas have been the primary goals of the program.
References
(1999). Making it Happen: Implementation Plan for Mental Health Reform Toronto: Ontario Ministry of Health. 49
(2001). Population of census divisions in Ontario. (Available from Statistics Canada) 36
American Psychiatric Association. (2000). Diagnostic and statistical manual of mental disorders (4th ed., text revision). Washington, DC: Author. 7
Andrews, G. & Whittchen, H. (1995). Clinical practice, measurement and information technology. Psychological Medicine, 25(3), 443-446. 27
Bigelow, D.A., Cutler, DL., Moore, L.J., McCoomb, P. & Lueng, P. (1988). Characteristics of state hospital patients who are hard to place. Hospital and Community Psychiatry, 39, 181-185. 27
Chamberlain, R., & Rapp, C.A. (1991). A decade of case management: a methodological review of outcome research. Community Mental Health Journal, 27, 171-188. 27
Eisen, S.V., Dill, D.L. & Grob, M.C. (1994). Reliability and validity of a brief patient-report instrument for psychiatric outcome evaluation. Hospital and Commnunity Psychiatry, 45, 242-247. 27
Endicott, J., Spitzer, R.L., Fleiss, J.L. & Cohen, J. (1976). The Global Assessment Scale: A Procedure for Measuring Overall Severity of Psychiatric Disturbance. Archives of General Psychiatry, 33, 766-771. 27
Gudeman, J.E. & Shore, M.F. (1984). Beyond deinstitutionalization: A new class of facilities for the mentally ill. New England Journal of Medicine, 311, 832-836. 27
Holloway, F. (1991). Case management for the mentally ill: looking at the evidence. International Journal of Social Psychiatry, 37, 2-13. 27
McGrew, J.H. & Bond, G.R. (1995). Critical ingredients of Assertive Community Treatment: Judgements of the experts. Journal of Mental Health Administration, 22, 113-125. 27
Overall, J. & Gorham, D. (1962). The Brief Psychiatric Rating Scale. Psychological Reports, 10, 799-812. 27
Solomon, P.S., Draine, J. & Delaney, M.A. (1995). The working alliance andn consumer case management. Journal of Mental Health Administration, 22, 126-134. 27
SPSS for Windows (Version 10.0.0) [Computer software and manual]. (1999). SPSS Inc. 22
Thompson, K.S., Griffity, E.E.H. & Leaf, P.J. (1990). A historical review of the Madison Model of community care. Hospital and Community Psychiatry, 34, 625-634. 27
Thornicroft, G. (1991). The concept of case management for long term mental illness. International Review of Psychiatry, 3, 125-132. 27
Trieman, N. & Leff, J. (1996). Difficult to place patients in a psychiatric hospital closure programme: the TAPS project 24. Psychological Medicine, 26, 765-774. 27
U.S. Department of Health, Education and Welfare. (1976). Clinical Global Impressions (ECDEU Assessment Manual for Psychopharmacology DHEW Publication No. (ADM) 76-338). Rockville, Maryland: Guy, W. (ed). 53
Wasylenki, D., Goering, P., Cochrane, J. et al. (2000). Tertiary Mental Health Services: 1. Key Concepts. Canadian Journal Of Psychiatry, 45, 179-184. 27
Corresponding author contact information:
Dr. Sandra Stewart
Northeast Mental Health Centre
P.O. Box 3010, Hwy. 11 North
North Bay, Ontario CANADA
P1B 8L1
Author Note
Oluboka, O.J., Stewart, S., Saltstone, M., Brown-Demarco, D., Deschenes, S., Wallace, D. and Adams, S. Northeast Mental Health Centre, North Bay Campus, North Bay, Ontario Canada.
O.J. Oluboka is now with the Department of Psychiatry, University of Calgary, Calgary, Alberta, Canada.
M. Saltstone is now at King & Saltstone, Associates in Practice, North Bay, Ontario Canada.
The PREP team acknowledges the contribution of the regional program managers of the Northeast Mental Health Centre, North Bay Campus and our partners in the northeastern Ontario community.
Copyright Priory Lodge Education Limited 2007
First Published December 2007
Click
on these links to visit our Journals:
Psychiatry
On-Line
Dentistry On-Line | Vet
On-Line | Chest Medicine
On-Line
GP
On-Line | Pharmacy
On-Line | Anaesthesia
On-Line | Medicine
On-Line
Family Medical
Practice On-Line
Home • Journals • Search • Rules for Authors • Submit a Paper • Sponsor us
All pages in this site copyright ©Priory Lodge Education Ltd 1994-


