Browse through our Journals...
One impact of the integrated care pathway on our service - NHS Tayside
Dr Moyra Guthrie, Consultant General Adult Psychiatrist. Murray Royal Hospital, Perth. PH2 7BH.
Dr Ziad Tayar, Speciality Registrar 5, Royal Dundee Liff Hospital, Dundee, DD2 5NF.
The past few decades have seen the introduction of a number of initiatives aiming to improve clinical effectiveness and thereby patient care, integrated care pathways are one of them. Integrated care pathways are structured multidisciplinary care plans which detail essential steps in the care of patients with specific clinical problems(1). They use multidisciplinary guidelines to implement clinical plans according to local best practice for different conditions. Integrated care pathways have been proposed as a new approach to patient care that fulfils many of the demands of modern medical care(2).
An integrated care pathway was introduced to the Mental Health Service in Tayside in 2006 and was gradually rolled out across the services. The integrated care pathway significantly changed the way multidisciplinary actions were recorded. Although a potential benefits of the integrated care pathways is to reduce documentations by recording only variation from the pathway(2); over the last few years, here in Tayside we have experienced increasing difficulties using the resulting new case record, which is significantly bigger in size than the old ones. From a practical point of view, more voluminous case notes have put a strain on the administration and medical record departments, particularly in terms of storage space and handling. However, of far more importance is the impact of the new system on clinicians, in terms of the accessibility of patient information during normal daily duties such as out-patient clinics, and particularly at times of emergency assessments. It seemed to us that there was far more paper for each episode of care and that the new case notes also appeared to us to cover shorter periods of time than the old notes did.
Given these impressions, we decided to investigate the matter further in a more objective way. Our choice of sample was influenced by our belief in the need to minimise the impact of fluctuations in the service input with our patient group over the study period, as well as the need to have case notes that cover sufficient periods of time before and after the introduction of the integrated care pathway to our service in the year 2006. We examined case notes of all ten patients from a General Adult rehabilitation unit at Murray Royal Hospital who had lengthy periods of inpatient care over the study period. Of the 10 patients we identified, six had continuous information to cover almost the whole period of their inpatient stay, those are whom we included in our study. The others having had significant periods of care in other areas within or outwith NHS Tayside.
The case notes were weighed using the same weighting scale and by the same person. We divided the weight of each file by the number of months it covers to determine the weight of paper work per month of care. The resulting data is shown in the two graphs below.
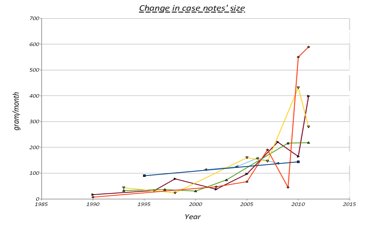
The first graph demonstrates the dramatic increase in size of case notes since 2006, the year the integrated care pathway was introduced to the service. Although the overall trend of change had been upwards before that, the speed and attitude of change is much bigger as of the year 2006 onwards. For example in the year 2000 the average weight of case notes per month per patient was around 50 grams, this figure jumped more than five fold to more than 250 gram per month per patient in 2010. Our impression that a year of care uses far more paperwork was correct.
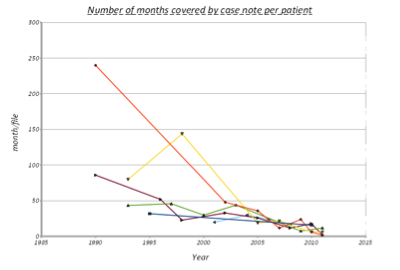
The second graph depicts the number of months covered by each volume of case notes per patient over time. Here we also witness a more marked reduction in this number since 2006-2007, when the ICP was introduced. Here again we see the number of months covered per case note per patient going down from around 60 in the year 2000 to around 10 in year 2012. Our impression that each set of notes covers a shorter period was also correct.
These findings have very important implications for clinicians who deliver care to individuals with complex long-term conditions. While the integrated care pathways are meant to improve multidisciplinary communication, and communication with patients(1)(2); the expand in the size of case record might lead to important historical information being buried in previous volumes of notes, and difficulties finding information will be exacerbated by the sheer volume of paper. In December 2007 NHS Quality Improvement Scotland published “Standard for Integrated Care Pathways for Mental Health” providing thirty nine standards for the implementation of Integrated Care Pathways. Of these, Standard 38 identifies the need for a multi-agency and multidisciplinary process for reviewing and analysing the variances gathered through regular review of the ICP to practice and service change. Standard 39 also stresses the importance of gathering stakeholder views on ICP care and recommends as a minimum an annual survey of staff, service users and informal carers to be completed and the results to be fed into the process of updating the ICPs(3).
The rationale behind using the Integrated Case Pathway is to improve the quality of care delivered to patients; however the complexity of the ICP paperwork might be counterproductive and defeating to its purpose. Our work has not looked into any change in the actual quality of care delivered before and after the introduction of ICP but rather was centred around the difficulties we encountered and which stem from the bigger and more complex Integrated Care Pathway paperwork. One could argue that the problem with the size and complexity of the new ICP would be less evident with an electronically based record keeping system.
This small project have confirmed our impressions of the impact the integrated care pathways have had on our service in terms of the practicality of handling the case notes and difficulties finding historical information within them. We believe more qualitative and quantitative research is required to assess the usefulness of the integrated care pathways and its impact of the service as a whole and more importantly on the quality of patient care.
References
1 Campbell H, Hotchkiss R, Bradshaw N, Poteous M. Integrated care pathways. BMJ 1998; 316: 133-137.
2 Kitchiner D, Bundred P. Integrated care pathways. Arch Dis Child 1996; 75: 166-168.
3 NHS Quality Improvement Scotland. Standards for integrated care pathways for mental health, 2007 (http://www.icptoolkit.org/adult_and_older_pathways.aspx).
Authors
Dr Moyra Guthrie, Consultant General Adult Psychiatrist. Murray Royal Hospital, Perth. PH2 7BH.
Dr Ziad Tayar, Speciality Registrar 5, Royal Dundee Liff Hospital, Dundee, DD2 5NF.
Copyright Priory Lodge Education Limited 2013
First Published January 2013
priory Useful links
Click
on these links to visit our Journals:
Psychiatry
On-Line
Dentistry On-Line | Vet
On-Line | Chest Medicine
On-Line
GP
On-Line | Pharmacy
On-Line | Anaesthesia
On-Line | Medicine
On-Line
Family Medical
Practice On-Line
Home • Journals • Search • Rules for Authors • Submit a Paper • Sponsor us
All pages in this site copyright ©Priory Lodge Education Ltd 1994-


