Browse through our Medical Journals...
Secondary Prevention of Stroke after Transient Ischaemic Attack: An Audit to review the medical management in a GP Surgery in the North West of England
Avraneel Talapatra, Medical Student, University of Manchester
Audit Supervisor: Dr Elizabeth Fiona Robertson MBChB, MRCGP, Diploma in Palliative Medicine(Distinction)
Abstract
Transient Ischaemic Attack (TIA) is an acute loss of focal cerebral or visual function lasting from several minutes to a few hours. TIAs of the anterior circulation have more serious prognosis than posterior circulation TIAs and may be amenable to Carotid surgery. However apart from immediate management following TIAs with ABCD2 scoring for risk stratification, Brain imaging, Carotid artery imaging and Aspirin 300 mg, adequate long term medical management is also necessary for secondary prevention of stroke and Myocardial Infarction. This involves antithrombotic treatment (or anticoagulation in atrial fibrillation with or without valvular lesions, valve prosthesis and dilated cardiomyopathy) together with control of hypertension, control of high cholesterol with statins and advice with regard to lifestyle measures. This audit was performed in our GP Practice to find out if these long term measures were being carried out adequately in patients with previous TIAs with or without Carotid Endarterectomy in accordance with the prevailing Guidelines in the United Kingdom. The aim was to ensure high quality of patient care following TIA and its improvement, if needed, in future.
Introduction
Statistical analysis shows that over 40,000 people in the UK suffer from TIA each year which enhances the risk of stroke (1). Stroke is responsible for 11% of all deaths in the UK and is the third biggest killer. It is also responsible for 5% of the total NHS budget. 15% of strokes are preceded by TIAs (2).
TIAs are temporary episodes of neurological dysfunction which usually last less than 24 hours. Notably, within 5 years, 1 in 6 patients suffer a stroke and 1 in 4 patients die from either stroke or heart attack (3).
TIAs are caused usually by micro-emboli often from AF, MI or valvular disorders. Reduced cerebral blood flow secondary to postural hypotension, cardiac arrhythmias or carotid artery stenosis may also cause TIA. Clinical presentations of anterior circulation or Carotid TIA commonly include hemisensory loss, hemiparesis, hemianopia, aphasia or Amaurosis fugax (2). They account for 80% TIAs and are associated with grave prognosis. Symptoms of posterior circulation or vertebro-basilar TIA comprise of diplopia, dysarthria, ataxia, bilateral weakness or abrupt bilateral cortical blindness (2,3).
Following initial management with Aspirin 300 mg daily, MRI brain, Carotid imaging and referral for carotid endarterectomy if warranted, the patients should have long term medical treatment to achieve cumulative risk reduction of vascular events by 80%, (4). This includes statins, antiplatelet agents, anticoagulants in atrial fibrillation, antihypertensives and proper advice with regard to dietary measures, quitting smoking and reduction of alcohol consumption (5-8). Secondary prevention following TIA, stroke and Carotid surgery is often suboptimal with most failing to achieve the targets and 15% continuing to smoke (4). The objective of this audit was to find out if the patients in the surgery who had TIA before were receiving the best possible ongoing medical management.
Aims
Based on the Guidelines of NICE (National Institute for Clinical Excellence), SIGN (Scottish Intercollegiate Network), GP Notebook and RCP (Royal College of Physicians) the audit was performed. The aims were as follows:
(1) To find out if those patients who suffered from TIA and not had carotid endarterectomy (CEA) were maintained adequately on antiplatelet agents, statins, antihypertensives and had advice to quit smoking and reduce alcohol consumption
(2) To find out if those who had CEA were receiving antiplatelets, statins, antihypertensives and received advice with regard to stopping smoking and decreasing alcohol consumption
The targets for post-TIA management were found to be different from each other in some areas in the different Guidelines. These include the drugs used and the blood pressure aims. Hence, it was decided to adhere to the NICE Guidelines primarily, with reference to the other available Guidelines as appropriate.
Criteria for Audit
(1) To find out if those with TIA and had no CEA were maintained on Aspirin and Dipyridamole (or Clopidogrel if the patients were allergic to Aspirin).
(2) To find out if the patients with previous TIA and who received medical management only were treated adequately with antihypertensive agents
(3) To find out if patients with previous TIA and who did not undergo CEA were receiving statins
(4) To find out if the above category of patients received advice with regard to smoking cessation and decreasing alcohol consumption
(5) To find out if post CEA, the patients received adequate medical management with antihypertensives
(6) To find out if post CEA, the patients received adequate medical management with statins
(7) To find out if post CEA, the patients received adequate management with Clopidogrel
(8) To find out if post CEA, the patients received adequate advice to quit smoking and decreasing alcohol consumption
The accepted standard of 90-100% was used for all of the criteria in this audit
Methodology
This was a retrospective audit where the data base of patients in our surgery with TIA were randomized into a total cohort of 50 patients (out of 136) using the website random.org and studied to find out if adequate medical management was done for secondary prevention of acute cerebral ischaemic event.
Literature review
The NICE Guidance (2008) on post TIA management was found to be most useful (5). Also, the summary of this guidance on GP notebook was quite valuable (7). The NICE guidelines were used as the primary resource on the topic because they are recommended by the UK Government. In addition, the RCP Stroke Guidelines (2012) and the SIGN (2008) Guidelines on post-TIA therapies were also looked into (6,8). Furthermore, the NICE Clinical Knowledge Summaries (NICE CKS, 2013) were also studied which provide primary care practitioners with a synopsis of the current evidence for different diseases. The Medline was also searched for meta-analyses and systems reviews.
1) Immediate management
Patients with suspected TIA should receive daily Aspirin 300mg immediately (5-8). The EXPRESS trial showed that early initiation of treatment measures in patients with TIA can reduce the risk of stroke within the next 3 months by 80% (9). As not all patients with TIA can be seen in clinic it is important to risk stratify patients using the ABCD2 score in order to predict the likelihood of future stroke (appendix 1).
All patients should be referred to a TIA clinic. If a patient has had two or more recent TIAs in the last week or has an ABCD2 score of 4 or more then they should also be admitted into hospital and investigations are usually carried out within 24 hours (5,7). If a patient has a score <4 in an isolated TIA then investigations are carried out over the next week. Patients usually undergo Echocardiogram. If the vascular origin of the pathology causing the TIA is unknown then Brain imaging is carried out ideally with diffusion weighted MRI scanning although CT scans are also used (5). This allows exclusion of intracranial haemorrhage.
Patients who present with symptoms of anterior circulation TIA often have carotid artery stenosis which may be amenable to surgery. All patients should have carotid ultrasound imaging within 1 week as per the NICE Guidelines (5). It is stated that a significant stenosis is when the patient has stable neurological symptoms and has stenosis of 50 to 99% according to NASCET (North American Symptomatic Carotid Endarterectomy Trial) Criteria or 70 to 99% according to ECST (European Carotid Surgery Trial) Criteria (10,11). These patients should be referred to Vascular surgery for Carotid endarterectomy (5). SIGN Guidelines suggest that males with internal carotid artery stenosis of 50 to 99% and females 70 to 99% should be referred for Carotid surgery (8). The combined risk of stroke and death following surgery is about 3% (2).
2) Long-term management
Long-term management involves the following categories:
a) Antiplatelet/anticoagulant therapy
b) Hypertension management
c) Cholesterol management
d) Lifestyle management
a) Antiplatelet/anticoagulant therapy
The PRoFESS trial from 2007 concluded that Aspirin and Dipyridamole MR or Clopidogrel are both associated with significantly improved outcomes in terms of subsequent stroke as compared to Aspirin monotherapy in patients post- TIA (12). However, the trial couldn’t conclude any one therapy as being significantly superior. According to GP Notebook and NICE guidance, patients with TIAs should be maintained on lifelong Aspirin 75 mg daily and Dipyridamole MR 200 mg twice daily as the first line treatment (7,13). If this is contraindicated then Dipyridamole MR alone is only recommended (7,13). The RCP Stroke Guidelines and NICE Clinical Knowledge Summary however suggest that Clopidogrel 75mg should be used as first line treatment for stroke prevention (6,14). Clopidogrel should be used as the first line drug following ischaemic stroke according to NICE Guidelines (13). The RCP guidance says that it should be assumed that TIA and stroke are part of the same pathology, so the same treatment should be used. Hence, the RCP recommends Clopidogrel as first line, then Aspirin and Dipyridamole MR as second line. If the patient is intolerant of both Clopidogrel and Dipyridamole then Aspirin monotherapy should be used for maintenance as third line (6). It was found that Clopidogrel had greater cost-effectiveness (6). However, for the purpose of this audit, I used mainly the NICE guidance and the GP Notebook which follows the NICE Guidelines as Clopidogrel is not currently licensed for use after TIA in the UK (13).
Anticoagulant therapy is recommended for patients with atrial fibrillation, prosthetic valves and dilated cardiomyopathy. Warfarin is used most commonly although the novel oral anticoagulants Dabigatran, Apixaban and Rivaroxaban can also be used except in cases of valvular heart diseases with AF. However where oral anticoagulation is contraindicated, an antiplatelet drug, such as Aspirin, may be appropriate (13).
b) Hypertension management
The SIGN guidelines suggest control of blood pressure to <140/85 mm Hg and <130/80 mm Hg in Diabetes (8). However, the RCP Guidelines instead recommend a target of < 130/80 mm Hg for all patients post-TIA (6). The Quality Outcomes Framework suggest a target of <150/90 mm Hg. I adhered to the RCP Guidelines in this case.
c) Cholesterol management
Patients should be started on a statin regardless of baseline cholesterol level. It is known statins significantly reduce risk of subsequent MI and also reduce risk of ischaemic stroke (5,6). The patient’s cholesterol levels should be rechecked after one to three months and if the total cholesterol is >4 mmol/L or LDL >2 mmol/L then dosage of statins should be increased (14).
d) Lifestyle and other measures
The blood sugar control should also be good (5,6). Proper advice with regard to dietary measures, quitting smoking and reduction of alcohol consumption (< 3-4 units/day in males and < 2-3 units/day in females) should also be given (6,8).
The criteria used in the audit differ from the Quality Outcomes Framework (appendix 2) with regard to the targets for blood pressure and cholesterol.
Results
Total number of patients- 50
Patients who had no CEA- 46
Males- 21; Females- 25
Age in years: 20-30- 1, 31-50- 1, 51-60- 7, 61-70- 7, 71-80- 17, 81-90- 12, 91-100- 1
No of patients who had CEA: 4
Males: 3; Females: 1
Age in years: 60-70- 1, 71-80- 3
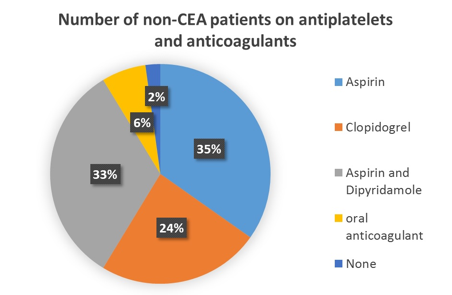
(1)Number of non-CEA patients on Aspirin and Dipyridamole- 15 out of 46(32.6%). Only Aspirin- 16 out of 46 (34.8%);
1 patient was on no antiplatelet agent (2.2%). This was a male patient aged 23 years.
(2) Number of non-CEA patients on Clopidogrel- 11 out of 46 (23.9%). There was no documented allergy to penicillin
(3) Number of non-CEA patients on oral anticoagulants- 3 out of 46(6.5%). These patients had AF, 2 were on Warfarin and 1 on Rivaroxaban
(4) Number of non-CEA patients on antihypertensives- 42 out of 46 (91.3%). No of patients with BP well controlled: 33, In 12 patients BP control was poor and in 1 patient there was no recent documentation of BP
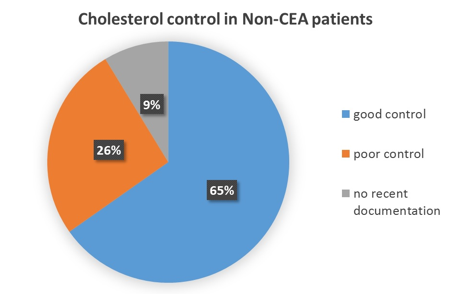
(5) Number of non-CEA patients on statins- 44 (95.7%). No of patients with total cholesterol<4 mmol/l and LDL< 2 mmol/l: 30, In 12 patients cholesterol was high and in 4 patients there was no recent documentation
(6) Number of non-CEA patients who received advice to quit smoking- All smokers were given advice to quit smoking. 3 patients still continued to smoke; 11 patients were ex-smokers; 31patients never smoked; no documentation in 1 patient
(7) Number of non-CEA patients who received advice to reduce alcohol consumption- 35
31 patients drink within permissible limits; 11 patients were lifelong teetotaller. Excessive drinker- 2; no documentation- 2
(8) Number of CEA patients on Clopidogrel- 2 out of 4. 1 was on Aspirin and 1 on Warfarin
(9) Number of CEA patients on antihypertensives - 4. No of patients with BP <130/80 mm Hg= 3
(10) Number of CEA patients on statins- 4. No of patients with Total Cholesterol <4 mmol/l and LDL < 2 mmol/l= 3
(11) Number of CEA patients who received advice to quit smoking- 3(1 never smoked). No patient smokes at present
(12) Number of CEA patients who received advice to reduce alcohol consumption- 3. 1 patient teetotaller
8 patients amongst the above population had Diabetes with HbA1c >7.5% (58mmol/mol) in 3 patients.

Report Analysis and Discussion
Patient demographics
TIAs are rare in young people without vascular risk factors. They are more common in men at relatively younger ages, but the sex difference reduces after the menopause. In our audit amongst the non-CEA patients out of 46, 21 (45.7%) were males and the remaining 54.3% were females and amongst those with CEA (4 in total), 3 (75%) were males and 25% females. Most patients were in the age group between 71-80 years, followed by the age group between 81-90 years in the non-CEA group. One young male patient suffered TIA. He was on Mirtazapine for depression. Mirtazapine is known to cause TIA (15).. Depression itself can predispose to stroke; one meta-analysis shows risk of stroke increases by almost 50% (16).
Antiplatelet or Anticoagulant therapy
According to the NICE Guidelines, following the initial treatment with Aspirin 300 mg for 14 days, Aspirin 75 mg daily and Dipyridamole MR 200 mg BD should be used for secondary prevention of Stroke following TIA (13). However the RCP Guidelines of 2012 and NICE CKS (revised in May 2015) suggest Clopidogrel as the first line drug for maintenance therapy (6,17).
According to NICE CKS in case of Ischaemic Stroke or TIA if Clopidogrel is contraindicated or not tolerated, then only a combination of Aspirin and Dipyridamole should be administered. Aspirin is to be given alone only if Clopidogrel or Dipyridamole is contraindicated (17). Our patients on Aspirin had no documented allergies to Clopidogrel or Dipyridamole. NICE CKS also recommends that in patients with multi-vascular disease (with history of TIA or ischaemic stroke and ACS) Clopidogrel should be the first line drug and Aspirin is to be used only if Clopidogrel is contraindicated (17).
Anticoagulants are used in AF, valve prosthesis and Dilated Cardiomyopathy. Novel oral anticoagulants however are not to be used in valvular AF. In TIA, the RCP Guidelines state that anticoagulation should be started immediately after haemorrhagic stroke has been ruled out with brain imaging. Anticoagulation should be continued without use of antiplatelet therapies.
Of the patients with no CEA (total 46), 16 patients (34.8%) were on Aspirin only. Most of these patients either suffered from Angina or had some form of Acute Coronary Syndrome in the past. 15 patients (32.6%) were on Aspirin and Dipyridamole and 11 patients (23.9%) were on Clopidogrel. This drug was started mostly in the hospital or TIA clinic. Another 3 patients (6.5%) were on anticoagulants; 2 were on Warfarin and 1 on Rivaroxaban.
According to our results a good number of patients were on Aspirin monotherapy despite evidence pointing towards its use alone being sub-optimal. As I decided to adhere to the NICE Guidelines in this case I could only count the 32.6% of patients on Aspirin and Dipyridamole to meet my audit criteria. However, as other Guidelines prefer Clopidogrel monotherapy as the first-line management it may be acceptable for the remaining patients to have this drug as an alternative. All of the patients with AF were on anticoagulation.
Although the NICE Guidelines aren’t specific about the choice of antiplatelet therapy post-CEA, the RCP Guidelines clearly state that Clopidogrel should be the first line drug (6). NICE CKS (revised in 2015) suggest in Carotid or Cardiac stenting, Aspirin 75 -300 mg is to be used in combination with any of the following drugs Clopidogrel 75 mg daily, or Prasugel 5-10 mg daily, depending on age and weight, or Ticagrelor 90 mg twice daily. This combination is to be used for 12 months followed by Aspirin life long (17). In our audit following Carotid Endarterectomy, out of 3 non-AF patients, 2 (66%) were on Clopidogrel and 1(33%) was on Aspirin. This shows most of these patients were following the RCP Guidelines.
Blood Pressure
According to the RCP Guidelines, all patients should be on antihypertensives following TIA and BP should be kept <130/80 mm Hg. A recent meta-analysis showed that reduction in BP by >10/5 mm Hg can decrease future stroke by approximately 30-40% (18). In our non-CEA group 42 out 46 patients (91.3%) were on antihypertensive agents. 33 patients (approximately 72%) had good BP control. All 4 patients with CEA were on antihypertensive agents and in 3 patients (75%) BP control was good. This shows that although we have met the standard target for putting patients on hypertensive medication, there is still room for improvement in BP control in 26% of the non-CEA patients and 25% of CEA patients.
Cholesterol
NICE Guidelines published in 2014 suggested for primary prevention a starting dose of Atorvastatin 20 mg daily in high risk cases and with a CVD risk of >10% over 10 years and for secondary prevention Atorvastatin 80 mg daily (19). The Guidelines published by JBS 2 (Joint British Society) mentioned that in high risk cases total cholesterol should not exceed 4 mmol/l and LDL should be less than 2 mmol/l and according to the JBS 3 Guidelines published in 2014 the shift of interest was more towards non-HDL, but they went on to mention that the LDL should not exceed 2 mmol/l in high risk cases (20). The audit standards included a total cholesterol of < 4mmol/l and LDL < 2 mmol/l. 44 patients (95.7%) were on statins and 30 (65%) patients had good cholesterol control. All 4 patients following Carotid endarterectomy were receiving statins with good cholesterol control in 75% cases. This shows that although the target was met for statin therapy, 26% of non-CEA and 25% of CEA patients could have improved cholesterol control.
Lifestyle
The Guidelines suggest that the safe limit of alcohol consumption is 3-4 units/day for males and 2-3 units/day for females (8). In the non-CEA group of the 46 patients, 11 were teetotaller (24%), 31 patients were drinking within safe limits (68%) and 2 patients were heavy drinker (4%). In another 2 patients there was no documentation of alcohol consumption. In the CEA group, of the 4 patients, 3 patients received proper advice and were drinking within safe limits, 1 patient was a teetotaller. This shows that the target for alcohol consumption post-TIA was met.
According to all Guidelines all patients should quit smoking following TIA (5-8). In the non-CEA group, all smokers were advised to quit smoking. However, 3 patients continued to smoke. In the patients following CEA all 3 patients (100%) who used to smoke before stopped smoking following advice to do so. This shows that the smoking cessation target was met.
5 out of 8 diabetic patients (61%) had HbA1c < 58 mmol/mol, but some of these patients are under secondary care for their diabetes. Although this wasn’t used as part of the criteria in our audit, this should be targeted by the practice.
Conclusion and Recommendations
Many patients with prior TIA go on to develop stroke. It is vital to provide patients with optimal secondary stroke prevention treatment. The Guidelines all aim to facilitate good practice; however, through the course of the audit I discovered that the targets are not always alike. I decided to mainly follow the NICE Guidelines here, but referred to the other available Guidelines, when appropriate, believing the Standards for the criteria of the audit to be between 90-100%. In the non-CEA group, a large number of patients were on Aspirin monotherapy with others were on Aspirin and Dipyridamole MR combination or Clopidogrel or anticoagulation for AF. All those who smoked received advice to quit it and all received advice regarding the safe limit of alcohol consumption. All patients with high BP were treated but it remained high in 12 patients. In the CEA group all were receiving either antiplatelet agents or Warfarin, statins and antihypertensives and received advice with regard to smoking cessation and safe limit of alcohol consumption. 3 out of 4 patients in this group had good BP control. Overall the performance of the Surgery was good, as indicated under the “Results” section, with most patients receiving ongoing medical care in accordance with the best practice and Guidelines available in the country
Recommendations
1. At the next monthly educational meeting, to discuss with the practice nurses, who carry out TIA clinics, the results of the audit and the latest Guidelines about antiplatelet, cholesterol, hypertension and lifestyle recommendations post-TIA
2. Invite the patients, not on optimal treatment post-TIA, to see the practice nurses to put them onto the best possible therapy
3. All patients who present to the TIA clinic and are on Aspirin monotherapy, BP higher than 130/80mmHg or LDL >2mmol/l should be given the appropriate optimal therapy including Aspirin and Dipyridamole combination, multiple anti-hypertensive agents and Atorvastatin 80 mg daily respectively
4. Patients who are still smoking or drink heavily should receive adequate advice about the risks of their behaviours and should be encouraged to quit smoking or reduce alcohol consumption.
5. The TIA register should be checked and patients who have not had their annual TIA review for over a year identified and be called for an annual check-up
6. All ongoing management in conformation with the Practice Guidelines should be clearly documented and any reasons for alteration of treatment should be stated.
7. Re-audit in a year to find out if there has been an improvement in our practice standards
Appendix 1: ABCD2 Scoring (3, page 174)
Age: 60 years or more-1 point; BP>140/90 mm Hg- 1 point; Clinical Features: Unilateral weakness- 2 points; Speech impairment without weakness- 1 point; Duration of TIA of 10-59 minutes-1 point; Duration of TIA >60 minutes- 2 points; Diabetes- 1 point
Appendix 2: QOF Criteria for TIA management.
(1) Indicator - Last BP in the preceding 12 months 150/90 mm Hg or less; Points-5; Achievement Thresholds- 40-75%
(2) Indicator- Record of total Cholesterol in the preceding 12 months; Points-2; Achievement thresholds- 50-95%
(3)Indicator- The above mentioned cholesterol is < 5 mmol/l; Points- 5; Achievement Thresholds- 40-65%
(4)Indicator- Anticoagulant or antiplatelet agent taken within the last 12 months; Points- 4; Achievement Thresholds-57-97%
References
1. Stroke Association (2015). State of the Nation: Stroke statistics. London: Stroke Association. Available at: https://www.stroke.org.uk/sites/default/files/stroke_statistics_2015.pdf
2. Jarman P. Neurological Disease. In: Kumar and Clark’s Clinical Medicine. Eds. Kumar P & Clark M. 8th ed., pp 1096-1099. UK: Saunders Elsevier Ltd; 2012.
3. Baliga RR. 250 cases in Clinical Medicine. 4th edn., pp173-175. UK: Saunders Elsevier, 2012
4. Johnson P, Rosewell M, James MA. How good is the management of vascular risk after stroke, transient ischaemic attack or carotid endarterectomy?. Cerebrovasc Dis 2007; 23(2-3):156-61
5. National Institute for Clinical Excellence. Stroke: Diagnosis and initial management of acute stroke and transient ischaemic attack (TIA). Clinical Guideline 68. London, NICE 2008. Available at: www.guidance.nice.org.uk/cg68
6. Intercollegiate Stroke Working Party. National Clinical Guideline for stroke, 4th edition. London: Royal College of Physicians, 2012. Available at: www.rcplondon.ac.uk/sites/default/files/national-clinical-guidelines-for-stroke-fourth-edition.pdf
7. GPnotebook. Secondary Prevention of stroke. Available at: http://www.gpnotebook.co.uk/simplepage.cfm?ID=x20110515182704270209
8. Scottish Intercollegiate Guidelines Network. Management of patients with stroke or TIA: assessment, investigation, immediate management and secondary prevention. National Clinical Guideline 108. Edinburgh: SIGN, 2008. Available at: http://www.sign.ac.uk/pdf/sign108.pdf
9. Fisher M, Lees K. EXPRESS Transient Ischemic Attack Study. Stroke. 2008; 39: 2400-01
10. Ferguson GG, Eliasziw M, Barr HWK, Clagett GP, Barnes RW, Wallace MC, et al. The North American Symptomatic Carotid Endarterectomy Trial. Stroke 1999; 30: 1751-58.
11. European Carotid Surgery Trialists' Collaborative Group. Randomised trial of endarterectomy for recently symptomatic carotid stenosis: final results of the MRC European Carotid Surgery Trial (ECST). The Lancet. 1998;351(9113): 1379 – 87
12. Diener HC. The PRoFESS trial: future impact on secondary stroke prevention. Expert Rev Neurother 2007; 7(9): 1085-91
13. National Institute for Clinical Excellence. Clopidogrel and modified-release dipyridamole for the prevention of occlusive vascular events. Technology Appraisal 210. London: NICE, 2010. Available at: www.guidance.nice.org.uk/ta210
14. National Institute for Clinical Excellence Clinical Knowledge Summary (2013). Stroke and TIA. Available at http://cks.nice.org.uk/stroke-and-tia#!references
15. Hansen RA, Gartlehner G, Lohr KN, Gaynes BN, Carey TS. Efficacy and safety of second-generation antidepressants in the treatment of major depressive disorder. Ann Intern Med 2005;143 (6): 415-26
16. Pan A, Sun Q, Okereke OI, Rexrode KM, Hu FB. Depression and risk of stroke morbidity and mortality: a meta-analysis and systematic review. JAMA 2011; 306(11): 1241-49
17. National Institute for Clinical Excellence Clinical Knowledge Summary (2015). Antiplatelet treatment. Available at http://cks.nice.org.uk/antiplatelet-treatment
18. Lawrence M, Pringle J, Kerr S, Booth J, Govan L, Roberts NJ, et al. Multimodal Secondary Prevention Behavioural Interventions for TIA and Stroke: a systematic Review and Meta-analysis. PLoS ONE 2015; 10 (3): e0120902. Available at : http://www.plosone.org/article/fetchObject.action?uri=info:doi/10.1371/journal.pone.0120902&representation=PDF
19. National Institute for Clinical Excellence. Lipid modification: cardiovascular risk assessment and the modification of blood lipids for the primary and secondary prevention of cardiovascular disease. Clinical Guideline 181. London: NICE, 2014. Available at http://www.nice.org.uk/guidance/cg181/chapter/1-recommendations
20. JBS Board. Joint British Societies’ consensus recommendations for the prevention of cardiovascular disease (JBS3). Heart 2014; 100(2): 1-67
First Published November 2015
Copyright 2015-
Click
on these links to visit our Journals:
Psychiatry
On-Line
Dentistry On-Line | Vet
On-Line | Chest Medicine
On-Line
GP
On-Line | Pharmacy
On-Line | Anaesthesia
On-Line | Medicine
On-Line
Family Medical
Practice On-Line
Home • Journals • Search • Rules for Authors • Submit a Paper • Sponsor us
All pages in this site copyright ©Priory Lodge Education Ltd 1994-


